Upper eyelid reconstruction can be challenging, as both the functional aspect of the eyelid wiper and the cosmetic appearance need to be acceptable. Replacing “like with like” often provides the most satisfactory outcome, particularly important when reconstructing the thin and hairless eyelid skin (1).
A blepharoplasty flap has been previously reported as a useful reconstruction approach for anterior lamellar defects lying between the lash line and the eyelid crease (2) and for medial pre-septal defects above the eyelid crease (3). This advancement flap utilizes the tissue that would normally be excised during blepharoplasty for the repair of anterior lamellar surgical defects (2).
We herein describe 3 cases with a variation of a blepharoplasty flap to suggest its use as an adjunct in the reconstruction of full-thickness lateral upper eyelid defects. This one-stage, non-bridging technique combines a free tarsal graft with a periosteal flap to reconstruct the posterior lamella. The anterior lamella is repaired utilizing the blepharoplasty advancement flap. It was applied to reconstruct 50% full thickness lateral upper eyelid defects where dermatochalasis exists, with good cosmetic and functional outcomes. This logical variation enables the reconstruction of significant defects using only local tissue, obeying the “like with like” principle, and helps avoid the need for a bridging flap. This case series has been reported in line with the PROCESS reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-21-62/rc) (4).
This study is a single-center, retrospective, consecutive case series. It was performed in accordance with the tenets of the Declaration of Helsinki (as revised in 2013) and was approved as a retrospective audit by our Institutional Review Board (Queen Victoria Hospital NHS Foundation Trust, UK; IRB-REF #528). Written informed consent was obtained from the patients for publication of this case series and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal. A retrospective chart review was conducted of consecutive cases performed by an experienced oculoplastics surgeon (ASL) in a tertiary oculoplastics referral center using the described technique between November 2017 and June 2020. All adult (>18 years) cases with lateral upper lid malignant lesions meeting the inclusion criteria (as described below) and that have undergone the described technique were included. Included subjects had at least six months of postoperative follow-up. Pre-intervention patient optimization (e.g., medication review and adjustment) was conducted in relevant cases.
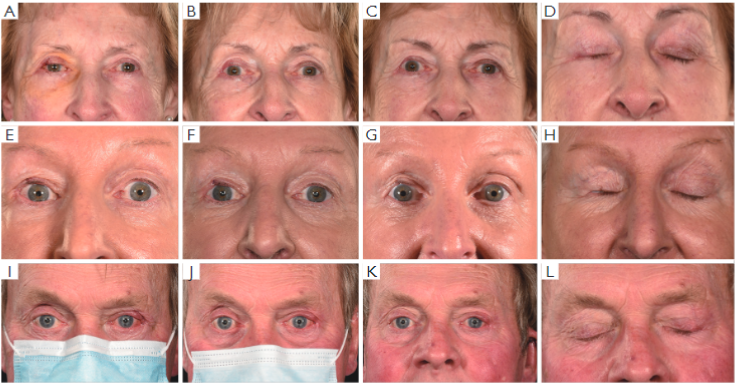
Reported outcomes were evaluated at 1–2 weeks, 4–8 weeks, and final follow-up (at least six months) and included complications (e.g., swelling, eyelid retraction, lagophthalmos, granuloma, infection, corneal epitheliopathy) and cosmetic results (e.g., eyelid contour, symmetry, scarring). All patients were clinically assessed by the senior author (ASL). Written consent for the use and publication of external photographs was obtained for each patient.
Following margin-controlled excision of a malignant eyelid tumor, the resultant defect is a full-thickness loss of the lateral ~50% of the upper eyelid (Figure 1A, Figure 2A). To utilize this approach, the vertical length from the superior edge of the defect to the inferior brow hairs must measure greater than 20 mm. This measurement corresponds to the residual lid margin to brow distance (LMBD) at the conclusion of the reconstruction, that is, following the advancement of the sub-brow flap to the newly created margin. If this criterion is met, a medial Burow’s triangle is marked by extending the upper edge of the defect (along the skin crease) towards the medial canthus (Figure 1B).
Firstly, the posterior lamella is reconstructed. The residual medial half of the upper tarsal plate is measured and is usually up to10 mm in height. The upper 4 mm of the tarsal plate is marked and taken as a free tarsal graft (Figure 1C). A tapering piece of tarsal plate is removed in order to preserve a minimum 5 mm tarsus over the key central corneal area. A typical graft may be up to 4 mm high, tapering to 1 mm medially, and approximately 10–15 mm long. The wider edge of the tarsal graft is sutured to the lateral edge of the existing tarsus using 5.0 Vicryl sutures (Ethicon, US), lining up the lower edges to recreate the lid margin (Figure 1D). At least two sutures should be placed to avoid buckling the tarsus and ensure correct alignment. Care must also be taken to ensure adequate bites of the tarsal plate while avoiding placing them at a full-thickness to prevent corneal injury. As the tarsal graft is likely to be insufficient to replace the entire posterior lamella, the remainder is reconstructed with a periosteal flap (Figure 1D,1E, Figure 2B). The authors prefer to create a vertical, inferiorly hinged transposition periosteal flap, which anchors inferiorly at the level of the lateral canthus of the lower lid. This way, the eyelid is suspended in an anatomical fashion and has the correct force vectors for a cosmetically pleasing postoperative lid appearance. The upper edge of the periosteal flap is sutured to the edge of the free tarsal graft using 1–2 bites of 5.0 Vicryl.
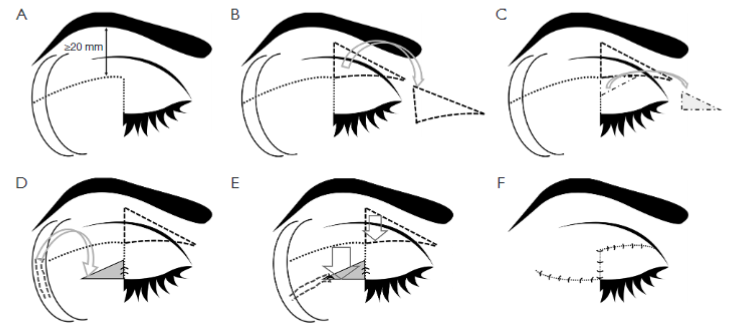
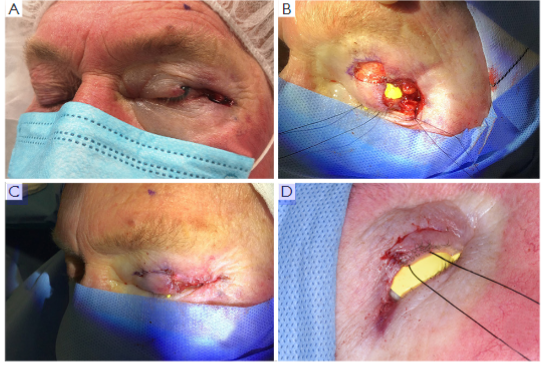
The anterior lamella reconstruction is then performed using a blepharoplasty flap, as described by McVeigh and Caesar (2). The previously marked medial Burow’s triangle is excised as a blepharoplasty overlying the medial lid remnant (see Figure 1B, Figure 2B). This is followed by extensive skin undermining of the lateral sub-brow advancement flap until this flap can be advanced downward to cover the reconstructed posterior lamella without tension (Figure 1E,1F, Figure 2C,2D). Any undue tension of the advancement flap is likely to cause a degree of lagophthalmos or eyelid retraction. If it cannot be moved easily, further undermining is required. Subcutaneous dissection is maintained, avoiding orbicularis oculi in order to minimize inadvertent denervation and postoperative lagophthalmos.
The skin advancement flap can then be placed with 6.0 sutures of choice (e.g., Vicryl Rapide, Ethicon). The new lid margin between the periosteal flap/free tarsal graft and the blepharoplasty advancement flap is sutured with a continuous 7.0 Vicryl suture. An antibiotic ointment is applied, followed by a pressure patch dressing overnight.
Others have described the use of a blepharoplasty flap for upper eyelid reconstruction. In 2003, Irvine and McNab (7) reported an approach to reconstructing central upper lid defects involving mobilization of residual tarsus and a type of blepharoplasty advancement flap. They described a local advancement flap utilizing the principles of upper blepharoplasty, and Burow’s triangles created medial and lateral to the flap. Good cosmetic results and minor complications were reported, including self-limiting edema and ptosis, irritation from lanugo hairs, and a minor degree of (asymptomatic) lagophthalmos. Then and Malhotra (3) described a superiorly hinged blepharoplasty flap utilizing a back-cut principle in patients undergoing medial upper eyelid xanthelasma excision. This technique negated the need for skin grafting and used pre-existing excess skin, resulting in good cosmesis (3).
In 2015, Allen (8) described in a video the use of an upper eyelid advancement flap utilizing a medial and lateral Burow’s triangles for the reconstruction of a central upper eyelid anterior lamellar defect. This video exemplifies the utilization of Irvine and McNab’s (7) type of blepharoplasty advancement flap for anterior lamellar defects. The blepharoplasty advancement flap, utilizing a medial Burow’s triangle, has previously been described by McVeigh and Caesar (2) when it was used to reconstruct the anterior lamella (without defect in the posterior lamella).
All these variations share common and logical principles, namely utilizing local advancement via principles of upper blepharoplasty and Burow’s triangles in individuals with dermatochalasis. Either medial or lateral (or both) to the defect, Burow’s triangles of skin are excised as blepharoplasty to allow inferior advancement of sub-brow skin. Only local tissue is exploited, and functional and aesthetic units are obeyed. The technique described herein highlights the blepharoplasty flap’s utility for lateral, full-thickness defects. Thus, joining these previous variations in representing an array of applications for the blepharoplasty advancement flap. Namely, for medial, central, or lateral; partial or full-thickness defects.
Lateral upper eyelid defects usually require more complex reconstructive techniques. Due to a lack of residual temporal tarsus, direct closure or the commonly used inverted semicircular “Tenzel flap" (9) are not options. Thus, eyelid sharing, or bridging, techniques are often employed and involve occlusion of the eyelid until the flap’s pedicle is divided (at a second stage) (10,11). One-stage non-bridging, non-occlusive techniques frequently involve using posterior lamellar grafts in combination with orbicularis mobilization (“sandwich flap”) and an anterior lamella graft (12,13).
The current technique provides a simple, one-stage option for flap reconstruction of the anterior lamella to allow grafting of the posterior lamella using an ipsilateral tarsal graft. This one-stage (non-bridging) technique should be advantageous to the traditional two-stage techniques in some patients (e.g., for those traveling from remote locations or with poor vision in the other eye). Using a transconjunctival graft provides the most similar tissue for posterior lamellar reconstruction and usually overlies the cornea to reconstruct larger eyelid margin defects. Using the blepharoplasty advancement flap for the anterior lamella potentially should offer the best outcome because of the identical tissue match and minimal contracture compared to skin grafts (1). Furthermore, ipsilateral use of tissue virtually eliminates secondary donor site morbidities.
The small number of patients in this series precludes any definite conclusions about outcomes with this reconstruction technique. Nonetheless, there was a rapid recovery of eyelid excursion and full closure within the first two weeks in all three patients. Acceptable eyelid contour and contralateral symmetry were also evident already at early follow-up. The resultant scarring was minimal. Thus, providing preliminary evidence of the potential of a good cosmetic outcome of upper lid appearance and contour, together with a fast recovery of appropriate eyelid function.
A potential complication of the current technique, even with appropriate patient selection (i.e., presence of sufficient dermatochalasis), is the development of some degree of flap contraction leading to a minor degree of lagophthalmos. In the series presented by Irvine and McNab (7), 1–2 mm of lagophthalmos was often present postoperative. Similarly, a 2 mm lagophthalmos developed between 5 weeks and three months postoperatively in one of our cases and was managed conservatively by daily massage and topical lubrication. The lagophthalmos improved with time, diminishing to 1 mm (mostly temporally), without symptoms or corneal epitheliopathy. We believe this may have occurred because some orbicularis muscle advancement occurred during skin advancement in this one case. Nonetheless, this should underscore the importance of patient selection, and proper measurement of the anticipated postsurgical LMBD should be performed in all cases. Furthermore, we believe that a generous sub-cutaneous undermining, leaving the orbicularis muscle undisturbed, and relieving any undue tension on the advancement flap, should help mitigate postoperative retraction and lagophthalmos.
Lastly, major reconstructions of the upper eyelid frequently result in the lack of eyelashes and occasionally eyebrows (1). When counseling patients regarding the option of utilizing this technique, they should be made aware that the reconstructed margin will lack eyelashes.
This study presents a novel technique for reconstructing large, full-thickness upper eyelid defects. It combines the use of a local tissue graft (tarsal) and flap (periosteal) for the reconstruction of the posterior lamella and the utilization of the blepharoplasty flap for the reconstruction of the anterior lamella. It thus provides a valuable option that spares the patient morbidity of a secondary donor site, the need for a secondary procedure and eye occlusion (e.g., when employing a bridging flap), and utilizes adequate local tissue (like-with-like principle). During patient selection, care should be taken to ensure sufficient residual eyelid skin (dermatochalasis). Intraoperative meticulous subcutaneous undermining of the eyelid skin flap should be performed to minimize postoperative contracture and lagophthalmos. Larger series with long postoperative follow-up are warranted to substantiate the favorable preliminary results reported herein.
Reporting Checklist: The authors have completed the PROCESS reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-21-62/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-21-62/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.