Background: Femtosecond laser astigmatic keratotomy (FSAK) and toric intraocular lens (IOL) implantation have been studied individually for comparison to treat astigmatism at cataract surgery. We report a case of surgically induced high corneal astigmatism by laser thermal keratoplasty (LTK) in a patient with cataract who was successfully treated with simultaneous combination of FSAK and toric IOL implantation with femtosecond laser-assisted cataract surgery (FLACS). This is the first report of both procedures combined simultaneously, with or without history of LTK.
Case Description: A 68-year-old male presented with a history of LTK with two enhancements each eye in 2004, with subsequent surgically induced high corneal astigmatism, and with age-related nuclear cataract of both eyes. IOL master demonstrated +7.71 diopters of astigmatism at 163 degree right eye and +3.29 diopters of astigmatism at 4 degree left eye. After extensive discussion of the risks and benefits, the patient agreed to undergo FLACS with FSAK with two 61 degrees of relaxation incisions (RIs) and toric IOL (Alcon SN6AT9) right eye; FLACS with toric IOL (Alcon SN6AT7) alone left eye. At 2-year follow-up, uncorrected visual acuity was 20/30 right eye, 20/25 left eye. His best corrected visual acuity was 20/25 (+0.25 +1.00 axis 21) right eye and 20/20 (plano +0.25 axis 90) left eye; his best corrected near visual acuity was J1+ with add +2.50 diopters right eye and left eye.
Conclusions: Patients with age-related cataract and LTK induced high corneal astigmatism can hardly be sufficiently treated with FSAK or toric IOL alone at the time of cataract surgery. An effective way is to combine large FSAK and toric IOL of the highest cylindrical power of T9, in our case, simultaneously, which can achieve an excellent long term visual outcome.
Laser thermal keratoplasty (LTK) is a technique to treat hyperopia (1) by applying localized heating of the corneal periphery to shrink collagen fibers leading to a complex alteration of the corneal surface and central corneal steepening (2). Surgically induced astigmatism by LTK has been reported (1,2).
Common surgical options for astigmatism include photorefractive keratectomy (PRK), laser-assisted in-situ keratomileusis (LASIK), small incision lenticule extraction (SMILE) and astigmatism correction along with cataract surgery. Astigmatic LTK was used to correct surgically induced astigmatism (+1.25 to +2.5 diopter of cylinder) by LTK (1); a 2-case report used LASIK to treat residual hyperopia and astigmatism after LTK (2); limbal relaxing incision (LRI) was performed on a patient with mixed astigmatism of +2.75 diopters in one eye and +3.0 diopters in the other eye after PRK and LTK (3). Literature on surgical treatment of high corneal astigmatism after LTK and cataract is rare.
We present a unique case of a 68-year-old male of high corneal astigmatism surgically induced by LTK and cataract who underwent a simultaneous combination of femtosecond laser astigmatic keratotomy (FSAK) and toric intraocular lens (IOL) with femtosecond laser-assisted cataract surgery (FLACS), which achieved an excellent long-term visual outcome. We present the following case in accordance with the CARE reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-22-15/rc).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A 68-year-old white male with a history of noninsulin-dependent diabetes mellitus, hypertension and high cholesterol, ocular history of LTK in 2004 with two enhancements each eye, high surgically induced astigmatism, with age-related nuclear cataract of both eyes presented for cataract evaluation for surgery. The patient reported no drug allergies and no significant family medical history and psycho-social history. He was on daily generic fluorometholone (FML) 0.1% suspension and Zadidor eye drops twice a day as needed for allergic conjunctivitis. His other medications included: Zolpidem (AMBIEN) 10 mg tablet at bedtime; amLODIPine-valsartan (EXFORGE) 5–320 mg daily.
His best corrected distance visual acuity was 20/40 (?1.75 +5.75 axis 161) right eye and 20/30 (+1.50 +2.75 axis 004) left eye; his best corrected near visual acuity was 20/40 (J3) (add +2.50 diopters) right eye and 20/30 (J2) (add +2.50 diopters) left eye. His best corrected visual acuity decreased to 20/200 each eye using the medium light setting of the Brightness Acuity Tester. External exam showed mild dermatochalasis bilaterally. Anterior segment examination revealed faint corneal LTK scars and surface irregularity of peripheral cornea bilaterally; 2+ nuclear sclerotic cataract in both eyes; otherwise negative. Dilated fundus exam showed a small choroidal nevus right eye, otherwise normal.
History of LTK in 2004 with two enhancements each eye followed by cataract evaluation; then underwent FLACS with FSAK and toric IOL implantation right eye and FLACS with toric IOL alone left eye in 2019, with postoperative follow-ups until 2021.
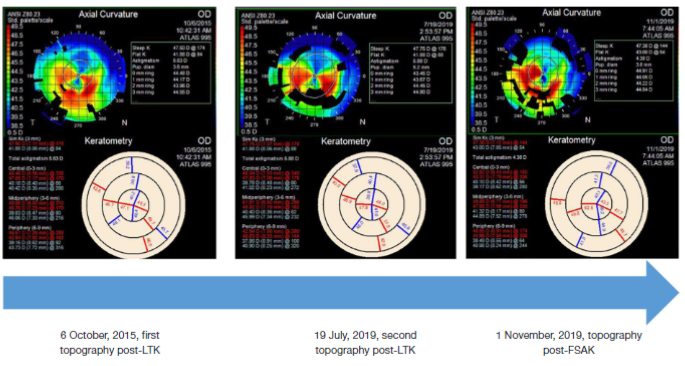
Topography showed high astigmatism with crab-claw like appearance in both eyes, photo was presented for the right eye (Figure 1). Repeated topography was stable a few years after (Figure 1). IOL master 700 (Carl Zeiss Meditec, Jena, Germany) demonstrated +7.71 diopters of astigmatism at 163 degrees right eye and +3.29 diopters of astigmatism at 4 degree left eye. Verion (Alcon, Fort Worth, TX, USA) demonstrated +6.89 diopters of astigmatism at 165 degrees right eye and +2.90 diopters of astigmatism at 7 degrees left eye.
Figure 1 Treatment timeline. (A) On 6 October, 2015, first post-LTK topography was obtained. High corneal astigmatism with crab-claw like appearance was present in both eyes, photo in the right eye was shown. (B) On 19 July, 2019, second post-LTK topography showed stable high corneal astigmatism in the right eye. (C) Reduced corneal astigmatism post-FSAK but still with crab-claw like appearance in the right eye. LTK, laser thermal keratoplasty; OD, oculus dextrus; FSAK, femtosecond laser astigmatic keratotomy.
After extensive discussion of the risks (including the difficulty to treat high cornea astigmatism at the time of cataract surgery) and benefits, the patient agreed to undergo FLACS with FSAK and toric IOL implantation right eye then FLACS with toric IOL alone left eye.
Informed consent was obtained and witnessed. The options of cataract surgery were discussed with the patient. The risks, benefits and alternatives were discussed in detail, including large residual astigmatism. The patient agreed to the risks, benefits and alternatives of the procedure.
Before surgery, the patient was treated with ofloxacin eye drops four times daily for 3 days, Ilevro eye drops once a day for 3 days, and 1% prednisolone eye drops four times daily for 3 days.
IOL power was determined by the Barrett TK toric formula of IOL master 700 with target reference of plano. Toric cylindrical power and axis were determined by the Alcon online toric IOL calculator and Verion surgical planning. The axis of the toric IOL of the right eye was found to be the same as the FSAK axis.
On the day of surgery, the patient received 1% tropicamide and 2.5% phenylephrine eye drops for pupillary dilation and proparacaine hydrochloride for topical anesthesia.
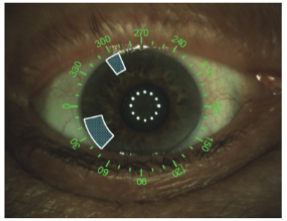
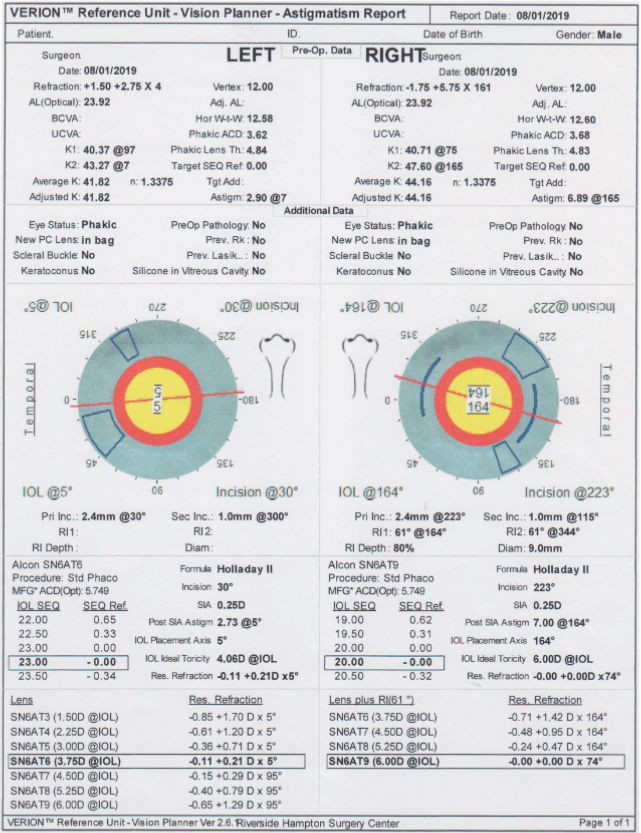
The patient was taken to the Lensx laser suite and attached to the usual monitoring devices by an anesthesiologist. Then the patient was placed in the proper surgical position under the laser. Data from the Verion reference unit (Figures 2,3) was transferred to the Verion digital marker to guide the procedure. The liquid optic interface was then applied to the sclera and docking was achieved. After manual verification of each procedural step, the Lensx laser was used to perform all of the following steps: astigmatic keratotomy (AK), i.e., relaxing incision (RI), capsulorhexis, and cataract fragmentation. Two 61 degrees of RIs in the right eye were 80% in depth and 9.0 mm in diameter at the axis of 164 degrees; no RI was necessary in the left eye.
After LenSx procedure, a Neuhann-Nuijts One Step Toric Marker was used to mark the toric axis at the patient’s sitting up position. Alcaine gel was then placed in the eye.
Figure 2 FSAK plan from the Verion reference unit of the right eye showed two 61 degree RIs at the axis of 164 degrees. Manual 2.4 mm primary incision at 223 degrees and 1.0 mm secondary incision at 115 degrees were also shown. FSAK, femtosecond laser astigmatic keratotomy; RIs, relaxing incisions.

Figure 3 Plan from the Verion reference unit of the left eye showed no RIs were necessary (toric IOL alone). Manual 2.4 mm primary incision at 30 degrees and 1.0 mm secondary incision at 300 degrees were shown. RIs, relaxation incisions; IOL, intraocular lens.
The patient was then brought to the operating room and prepped and draped in the usual fashion. A lid speculum was placed in the operative eye. The paracentesis was created with supersharp followed by instillation of 1% preservative-free lidocaine and epinephrine followed by viscoat viscoelastic (Alcon). The main clear corneal incision was then created with a keratome. Forceps were used to remove the anterior capsule of the laser capsulotomy. Hydrodissection was then achieved with balanced salt solution (BSS). The phacoemulsification tip was then placed into the anterior chamber and the pre-fragmented lens nucleus was removed. The irrigation/aspiration (I/A) device was used to remove any additional cortical material. The aphakic eye was then filled with provisc viscoelastic (Alcon) and Verion digital marker (which was consistent with AK axis and manual marking) was used to confirm the axis of the toric IOL. The toric IOL was then injected into the capsular bag and rotated in the position as indicated by the Verion digital marker. The I/A device was used to remove any remaining viscoelastic material. The wound edges were hydrated with BSS. A 0.1 mL aliquot of preservative free Vigamox was injected intracamerally. At the end of the procedure the wound was watertight, pupil was round and IOL in good position with excellent centration and approximately 1 mm overlap of the edge with the anterior capsule. One drop of 1% prednisolone was put into the eye. The lid speculum was removed. Protective sunglasses were then placed onto the patient. The patient was taken to the post anesthesia care unit (PACU) in stable condition having tolerated the procedure.
After the surgery, the patient was treated with ofloxacin eye drops four times daily for 7 days, Ilevro eye drops once a day until running off, and 1% prednisolone eye drops four times daily for 7 days, then three times a day for 7 days, then twice daily for 7 days, then once daily for 7 days then off.
For the right eye, at postoperative day 1, uncorrected visual acuity was 20/50, pinhole to 20/30; at postoperative week 1, uncorrected visual acuity was 20/20, toric IOL was in good position. For the left eye, at postoperative day 1, uncorrected visual acuity was 20/30; at postoperative week 1, uncorrected visual acuity was 20/25, toric IOL was in good position.
At postoperative week 11 of the right eye, which was postoperative week 8 of the left eye, his uncorrected distance visual acuity was 20/30 right eye, 20/25 left eye; his uncorrected near visual acuity was J2 right eye and J2 left eye. His best corrected distance visual acuity was 20/20 (?0.25 +2.00 axis 20) right eye and 20/20 (+0.50 sphere) left eye; his best corrected near visual acuity was J1+ with add +2.50 diopters both eyes.
Postoperative topography of the right eye was obtained at week 11 and showed decreased corneal astigmatism but still with crab-claw like appearance (Figure 1).
At 1-year follow-up, uncorrected visual acuity right eye was 20/25, left eye 20/20. His manifest refraction was +0.25 +1.00 axis 10 visual acuity 20/20 right eye, plano +0.25 axis 90 visual acuity 20/20 left eye.
At 2-year follow-up, uncorrected visual acuity was 20/30 right eye, 20/25 left eye. His best corrected visual acuity was 20/25 (+0.25 +1.00 axis 21) right eye and 20/20 (plano +0.25 axis 90) left eye; his best corrected near visual acuity was J1+ with add +2.50 both eyes. Toric IOLs remained in good position in both eyes.
There were no adverse and unanticipated events.
Our patient was successfully treated with a novel combined simultaneous FSAK and the toric IOL implantation. Both techniques have been studied individually for comparison to treat astigmatism at cataract surgery (4,5). This is the first report of both procedures combined simultaneously, with or without history of LTK.
Different techniques can be used to correct corneal astigmatism in cataract surgery, peripheral corneal relaxing incisions (PCRIs) and toric IOLs have been the two main options for astigmatism management during cataract surgery (6). The advantages of FSAK over conventional methods have been recognized, including almost no risk of infection, wound gape, and epithelial ingrowth (7). A prospective interventional case series showed that combined FLACS and FSAK may be an effective approach to manage preoperative astigmatism in cataract surgery (8). However, it limits to 1 to 3 diopters and slight under correction may exist during short-term follow-up (8).
The AcrySof Toric IOL (Alcon) is designed to correct corneal astigmatism ranging from 0.67 (T2) to 4.11 (T9) diopters (D) (9). While AMO Tecnis Toric IOL, Toric IOL II (Abbott Medical Optics, Inc., Santa Ana, CA, USA) is designed to correct corneal astigmatism ranging from 1.03 [150] to 4.11 [600] diopters. To correct high corneal astigmatism (in our case +7.71 diopters in the right eye), neither FSAK nor toric IOL alone is sufficient.
Sorkin et al. (10) reported stepwise combination of FSAK with phacoemulsification and toric IOL implantation in treatment of very high postkeratoplasty astigmatism. In these cases, the FSAK was performed first and not simultaneously with toric IOL. This stepwise approach was relatively safe however not so convenient for the patients.
In our patient, the IOL online toric IOL calculator showed an anticipated residual refractive astigmatism magnitude of 3.79 diopters and axis at 164 degrees with the highest cylindrical power of toric SN6AT9 (Figure 4). We hypothesized that the simultaneous combined procedure would have additive effect and could sufficiently treat this high astigmatism. This was supported by the surgical planning from the Verion reference unit with residual refraction of 0 diopter cylinder combining SN6AT9 and two RIs of 61 degrees (Figure 5). At postoperative day 1, the patient’s visual acuity without correction was 20/50; at postoperative week 1, visual acuity without correction significantly improved to an excellent 20/20 with good quality of vision, with toric IOL at nicely oriented position. Topography at postoperative week 11 did show partially corrected corneal astigmatism by large FSAK (Figure 1), and residual high astigmatism was neutralized by toric IOL T9. At 2-year follow-up, the patient’s uncorrected visual acuity remained at 20/30.
Figure 4 The IOL online toric IOL calculator of the right eye showed an anticipated residual refractive astigmatism magnitude of 3.79 diopters and axis at 164 degrees with the highest cylindrical power of toric SN6AT9. IOL, intraocular lens; OD, oculus dextrus; SE, spherical equivalence; K, keratometry; SIA, surgically induced astigmatism.
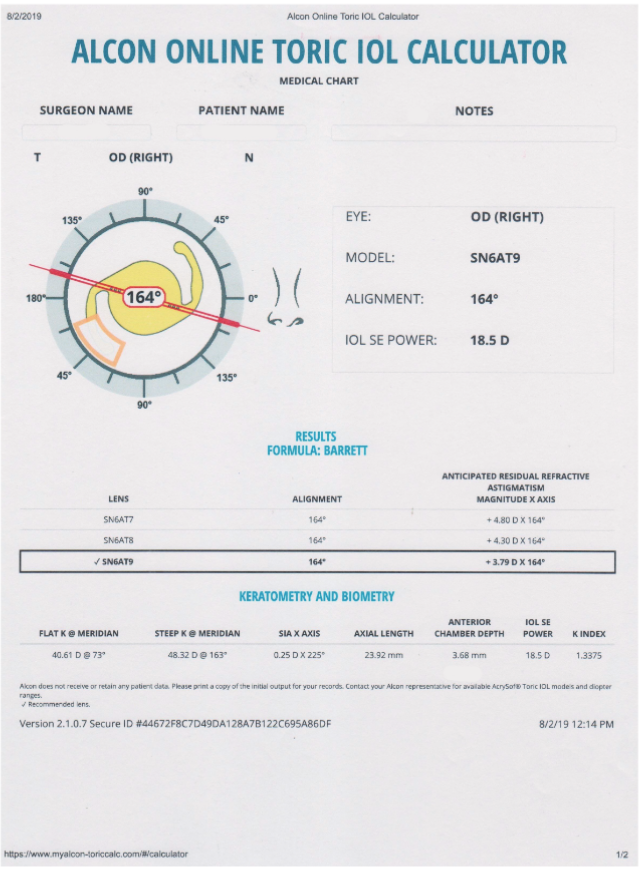
Figure 5 Surgical planning from the Verion reference unit showed residual refraction of 0 diopter cylinder when combine toric IOL of SN6AT9 and FSAK of two RIs of 61 degrees of the right eye. FSAK, femtosecond laser astigmatic keratotomy; Hor W-t-W, horizontal white to white; Lens th, lens thickness; SEQ, spherical equivalence; IOL, intraocular lens; MFG*ACD, manufacturer listed A constant; SIA, surgically induced astigmatism; RI, relaxation incision; Res. Refraction, residual refraction.
In summary, we describe the simultaneous use of large FSAK and the toric IOL T9 in treating LTK induced high corneal astigmatism. At the time of cataract surgery, this simultaneous combined procedure can effectively reduce high corneal astigmatism not able to be corrected by either individual procedure alone and achieve an excellent long term visual outcome. This is more convenient than the stepwise approach.
Limitation of the study is that this is a case report of the treatment of high cornea astigmatism after LTK at the time of cataract surgery. The risk of undercorrection or overcorrection with the simultaneous approach is relatively high. With this approach, a detailed and extensive discussion with the patient with a total understanding of the potential unpredictable refractive outcome should take place. Even it is more convenient for the patient with the simultaneous approach, an alternative and relatively safer stepwise approach should present to the patient. In this case report, we showed a successful outcome, however, case series of simultaneous FSAK and toric IOL will further demonstrate the effectiveness of the combined surgeries in treating high cornea astigmatism.
The patient expressed immediate satisfaction of the surgical outcome on postoperative day 1 after each eye surgery. Contentment was revealed in all of his follow ups as well. He was pleased with the smooth recovery. After the surgery, the patient had a significant decrease of the need for glasses. He rarely used his glasses for distance vision and only used his glasses for near vision for small prints at dim light. An overall good quality of vision was reported by the patient.
We thank the patient who participated in this study. We also thank the staff members at Hampton Roads Eye Associates, Hampton Surgical Center, Riverside Medical Group, Hampton, Virginia for their support.
Funding: None.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-22-15/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-22-15/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.