Introduction
Bacillary layer detachment (BALAD) is a recently-described phenomenon characterized by the accumulation of fluid at the inner photoreceptor segment myoid level, proximal to the external limiting membrane (ELM). This finding has been found in patients with diverse primary diagnoses which share the common feature of serous exudation in the posterior pole. However, thus far there have been few reports in the literature of BALAD in patients with posterior scleritis (1-3).
Here we present a case of idiopathic unilateral posterior scleritis presenting with BALAD associated with rapid vision loss. The patient responded to high dose systemic steroids with near complete restoration of the retinal architecture and recovery of vision.
This case provides further evidence that posterior scleritis can be a cause of BALAD. The rapid presentation and excellent visual and anatomical outcome of this case is entirely consistent with known descriptions of BALAD in a variety of other conditions (3,4). In conjunction with other recent literature (4-6), this case supports the categorization of BALAD as an entity distinct from other forms of intraretinal fluid, retinal detachment, and retinoschisis. We present the following article in accordance with the CARE reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-21-61/rc).
Case presentation
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A 16-year-old male with no significant prior medical or ocular history presented to the emergency department complaining of right-sided eye pain, blurry vision, and ptosis. He had initially noticed vision changes and pain upon awakening the morning 5 days prior to presentation. He described his visual changes as a dark spot in his central vision that waxed and waned. He was ultimately brought to the emergency department after his father noticed a new right eyelid droop.
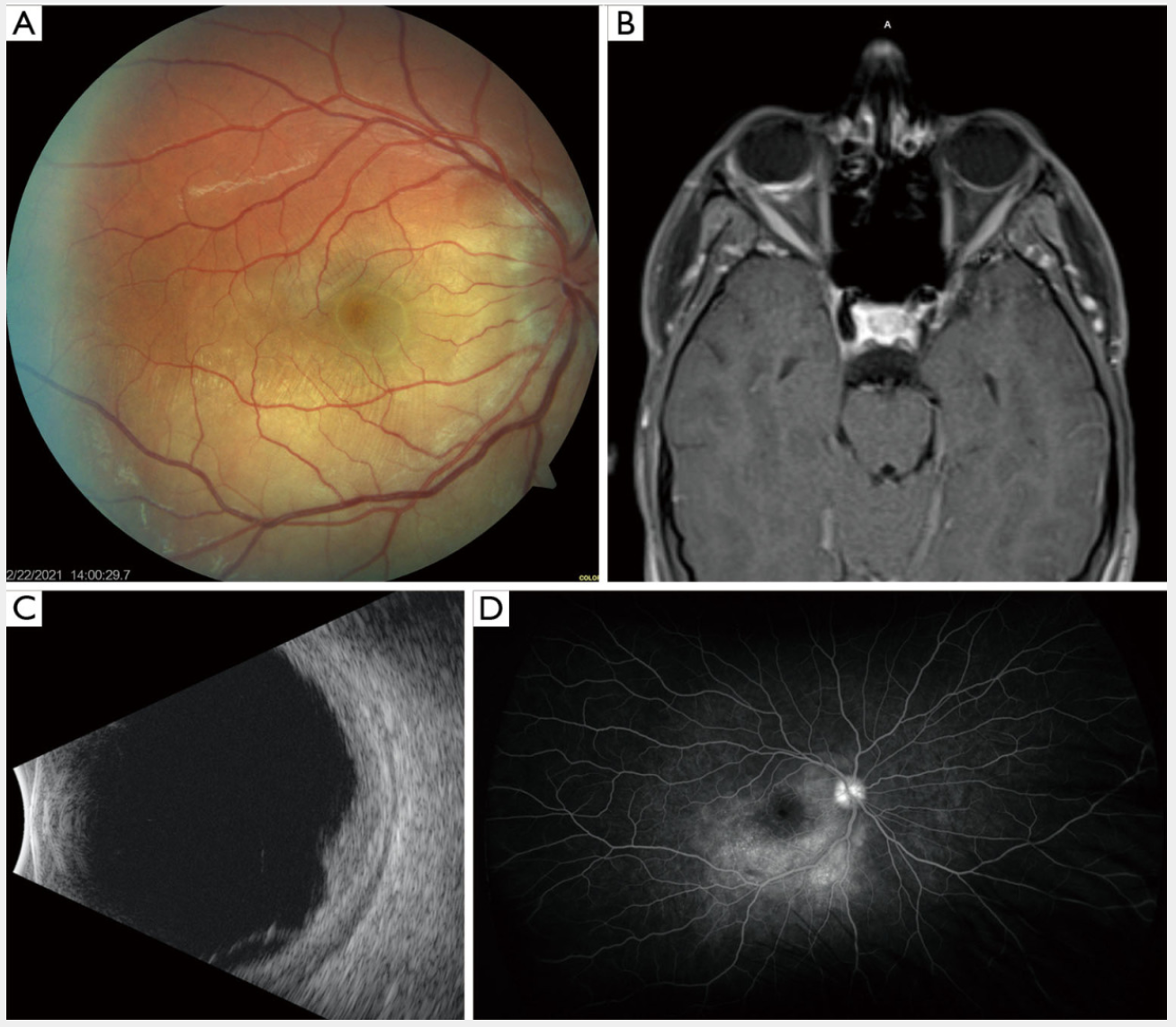
On initial exam, he was found to have a 1–2-mm right upper eyelid ptosis and decreased visual acuity to 20/70 in the right eye, with 20/20 vision in the left. On funduscopic exam, he had right optic nerve edema without hemorrhages or pallor as well as macular edema and dependent subretinal fluid (Figure 1A). The retinal periphery appeared normal. Funduscopic examination of the left eye was normal. He was admitted for further evaluation. Magnetic resonance imaging (MRI) of the brain and orbits did not reveal any tumors or brain lesions but was significant for a focal T1 enhancement of the right posterior globe (Figure 1B). Magnetic resonance arteriography/magnetic resonance venography (MRA/MRV) of the brain did not show any vascular abnormalities or lesions.
Figure 1 BALAD in a case of posterior scleritis. (A) Fundus photograph of the right eye. (B) T1-weighted MRI of the brain and orbits demonstrating focal enhancement of the right posterior globe. (C) B-scan ultrasound of the right eye. (D) Fluorescein angiogram of the right eye 5 days after initial presentation. BALAD, bacillary layer detachment; MRI, magnetic resonance imaging.
A B-scan ultrasound of the right eye showed choroidal thickening, subretinal and subtenon fluid, but no focal lesion or tumor (Figure 1C). Fluorescein angiogram showed optic nerve hyperfluorescence and punctate leakage throughout the macula without vasculitis, most consistent with a posterior scleritis (Figure 1D).
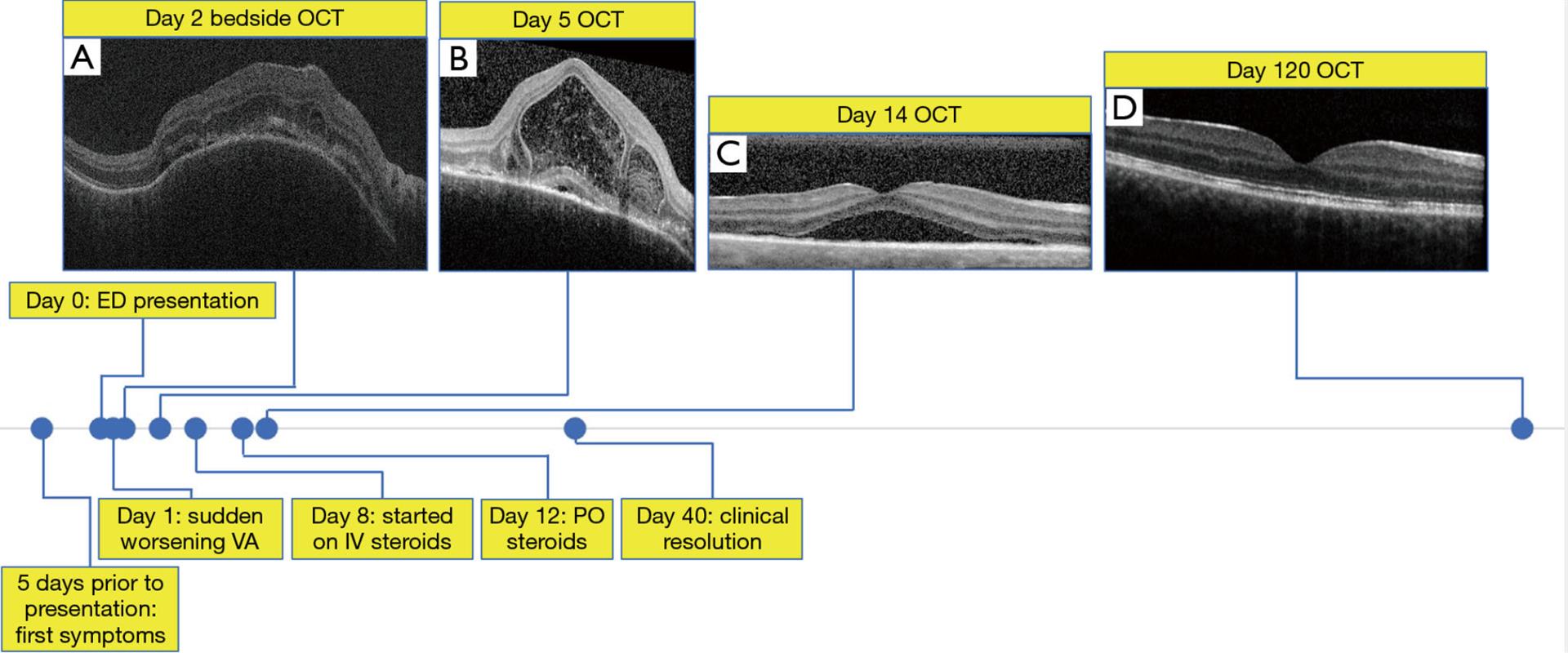
The patient noted sudden worsening of his vision symptoms his visual acuity was reduced to 20/400 in the right eye, along with a new right-sided relative afferent pupillary defect. Bedside optical coherence tomography (OCT) the following morning showed multifocal pigment epithelial detachments, edema of the retinal pigment epithelial layer (RPE) and hyperreflective curvilinear structures in the outer retina, reminiscent of outer retinal tubulation (ORT) surrounding dome-shaped hyperreflective material in the subretinal space (Figure 2A). Three days later the patient was seen in clinic. OCT showed progression of RPE and retinal detachments, with accumulation of dome-shaped layered hyperreflective material and punctate hyperreflective material in the subretinal space (Figure 2B).
Figure 2 Timeline of the case labeled with key events and select OCT imaging; all images are the macula of the right eye. (A) Portable OCT of the macula performed at bedside on day 2 after initial presentation. (B) OCT of the macula 5 days after initial presentation demonstrating splitting of the myoid zone separating the ELM from the ellipsoid zone. (C) OCT of the macula after 1 week on high-dose steroids. (D) OCT of the macula 4 months after initial presentation. ED, emergency department; ELM, external limiting membrane; IV, intravenous; OCT, optical coherence tomography; PO, oral; VA, visual acuity.
Infectious workup, including rapid plasma reagin (RPR), tuberculosis testing, HIV testing, and serum antibody testing for Treponema, Bartonella, Rickettsia, Blastomyces, Histoplasma, Toxocara, Toxoplasma, varicella-zoster virus (VZV), Epstein-Barr virus (EBV), and Lyme disease were all negative. Herpes simplex virus (HSV) 1 IgG was positive, but serum HSV PCR was negative. Rheumatoid factor, anti-nuclear antibodies, anti-neutrophilic cytoplasmic antibodies, erythrocyte sedimentation rate, C-reactive protein levels and angiotensin converting enzyme levels were also all within normal limits.
The patient was treated with 500 mg intravenous methylprednisolone twice daily for 3 days followed by 80 mg (1 mg/kg) per day of oral prednisone for 1 week. His pain and ptosis resolved and by 1 week after initiation of steroids the RPE detachments had resolved and his subretinal fluid was reduced (Figure 2C). His prednisone dose was gradually tapered down to zero over the course of 2 months. He experienced no adverse or unanticipated events from treatment. By 5 weeks after his initial presentation, all intraretinal and subretinal fluid had resolved without the appearance of retinal exudates. He experienced a gradual improvement in his visual acuity to 20/20 over the course of 4 months. Repeat fundus exam at 4 months after his initial presentation showed only abnormal foveal retinal pigmentation, with subtle irregularity of the RPE and photoreceptor layers seen on OCT (Figure 2D).
Discussion
In summary, we present a case of a child with acute posterior scleritis associated with the accumulation of fluid visible between the ELM and the ellipsoid band on OCT. This splitting, which likely occurs within the myoid level of the inner photoreceptor segments, is a finding that has been recently termed “bacillary layer detachment”, or “BALAD” (4-6). Previous studies have described BALADs extensively in patients with choroidal neovascularization, ocular toxoplasmosis, Vogt-Koyanagi-Harada (VKH) disease, exudative age-related macular degeneration, and acute posterior multifocal placoid pigment epitheliopathy (7-9). Ramtohul et al. (4) recently published an exhaustive literature review of case reports with OCT findings consistent with BALAD and found only three documented cases of BALAD associated with posterior scleritis (1-3). To our knowledge, the case report by Inan et al. (2) is the only previously documented case of BALAD in a pediatric patient with posterior scleritis. Our case expands the list of clinically documented bacillary detachments and adds to the body of evidence that posterior scleritis can result in this interesting finding.
Cicinelli et al. (3) hypothesized that in these cases acute fluid shifts in the posterior pole may force fluid into the neuroretina via hydrostatic pressure, causing a splitting within the photoreceptors due to shearing forces. Interestingly, posterior scleritis is commonly associated with scleral edema and specifically with fluid buildup within Tenon’s space. Our patient’s clinical course included an acute overnight worsening in his visual acuity several days following his initial symptoms. We hypothesize that this worsening may correspond to a rapid retinal fluid shift, consistent with the conclusions of Cicinelli et al. (3). In our patient, focal posterior scleritis lead to BALAD, however, the multiple case reports of BALAD associated with VKH reveal that a diffuse choroidopathy can also lead to focal BALAD.
Ramtohul et al. (4) postulate that accumulation of subretinal fibrin may disrupt adhesion between photoreceptors and RPE cells, increasing the likelihood of fluid entry into the myoid zone layer and therefore leading to BALAD under hydrostatic conditions that would otherwise lead to serous retinal detachment. Support for this argument notes that fluid within the BALAD cavity frequently includes suspended hyperreflective particles, not commonly found in subretinal fluid, likely representing inflammatory products, including fibrin, as well as photoreceptor debris. Our patient’s OCT (Figure 2B) also demonstrated accumulation of dome-shaped layered hyperreflective material and punctate hyperreflective material in the subretinal space, consistent with this hypothesis.
Previously published reports of BALAD also have noted that patients have generally had relatively rapid restoration of outer retinal architecture and were able to regain visual acuity following resorption of retinal fluid (3,4). This was also the case for our patient, who had significant improvement in his OCT and in his visual acuity at within a few months of steroid administration. We hypothesize that the retinal pigmentation observed on fundoscopy at his follow-up visit represents RPE hyperplasia resulting from his severe BALAD.
Despite the ubiquity of modern OCT imaging in retinal diagnosis, only recently has BALAD become a recognized manifestation of intraretinal and subretinal fluid. While there have been only a few case reports of BALAD associated with posterior scleritis, these cases have had many features in common with other documented cases of BALAD. This supports the hypothesis that, relative to other forms of retinal detachments and retinoschisis, BALAD has distinct etiology and prognosis. This interesting OCT finding undoubtedly merits more widespread recognition and further study.
Acknowledgments
Funding: This work was supported by an unrestricted grant to the Department of Ophthalmology and Visual Sciences from Research to Prevent Blindness.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ajay Singh and Jay M. Stewart) for the series “Medical and Surgical Challenges in Retina” published in Annals of Eye Science. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-21-61/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-21-61/coif). The series “Medical and Surgical Challenges in Retina” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.