Abstract: Anthropometry can analyze the size, weight, and proportion of the human body objectively and quantitatively to supplement the visual assessment. Various non-invasive three-dimensional (3D) anthropometric techniques have been applied to assess soft tissues’ 3D morphology in the clinical practice. Among them, non-invasive stereophotogrammetry and laser scanning techniques are becoming increasingly popular in craniofacial surgery and plastic surgery. They have been applied for craniofacial growth estimation and morphometric investigation, genetic and acquired malformation diagnosis, as well as orthodontic or surgical treatment arrangement and outcome evaluation. However, few studies have been published for assessing the 3D morphology of soft tissues in the periorbital region. This paper reviews the studies involving the application and evaluation of the increasingly popular 3D photogrammetry in the periorbital region. These studies proposed detailed and standardized protocols for three-dimensionally assessing linear, curvilinear, angular, as well as volumetric measurements, and verified its high reliability in the periorbital region (even higher than caliper-derived direct measurements). In the future, reliable and accurate 3D imaging techniques, as well as standardized analyzing protocols, may find applications in following up morphological growth, preoperatively diagnosing and assessing patient periorbital conditions, planning surgical procedures, postoperatively evaluating treatment outcomes of a specific procedure, and comparing the differences in surgical results between various procedures, studies, as well as populations.
Anthropometry can analyze the size, weight, and proportion of the human body objectively and quantitatively to supplement the visual assessment (1). Many scientific fields have employed anthropometric data for various aims, especially in craniofacial surgery, breast plastic surgery, and oculoplastic and reconstructive surgery (2-4). Anthropometry of the craniofacial soft tissue plays an essential role in the clinical practice by measuring various parameters between landmarks defined on the head, face, and ears. It can be applied for craniofacial growth estimation and morphometric investigation, genetic and acquired malformation diagnosis, as well as orthodontic or surgical treatment arrangement and outcome evaluation (5-7).
However, few studies have been published for assessing the 3D morphology of soft tissues in the periorbital region. Therefore, this paper aims to review the application and evaluation of the increasingly popular three-dimensional (3D) photogrammetry in the periorbital region. In this study, a PubMed database search was performed to identify relevant publications using the search algorithm [(photogrammetry) AND (three-dimension*)] AND [(eye) OR (face)]. We also screened relevant research missed in this search algorithm from the reference lists of specific full-text papers. After looking through these papers, we summarized the landmarks when measuring the periorbital region three-dimensionally and included the typical studies.
Traditionally, craniofacial anthropometry is mainly obtained by direct anthropometry and two-dimensional (2D) photogrammetry or cephalometry. However, people are increasingly aware of their disadvantages. These technologies cannot completely capture and quantify the complex 3D craniofacial morphology of the human (8). Besides, the direct technique demands massive measuring time, close physical contact, and excellent patient compliance; 2D photogrammetry lacks proper 3D morphological depth (9); cephalometry exposes the subjects to hazardous ionizing radiation.
To date, various non-invasive 3D capture and quantification techniques have been applied in the clinic practice, e.g., magnetic resonance imaging, quantitative ultrasound, laser scan, and stereophotogrammetry. Knoops et al. (10) compared the properties of four 3D scanning systems, including the 1.5T clinical MR Avanto Scanner, the static 3dMDface System, the handheld M4D Scan, and the Structure Sensor. They concluded that the 3dMDface System and M4D Scan supply high-quality results; the scanner choice is up to clinical and technical requirements; compact, handheld 3D systems would become increasingly popular in the near future.
Compared with traditional 3D techniques, laser scanning and stereophotogrammetry are highly accurate and precise, rapid and straightforward, and non-invasive. Besides, they can quantify various parameters, including linear distances, curvatures, angles, volumes (11), and surface areas (10). In contrast to laser scanning technique, stereophotogrammetry captures high-resolution 3D surface images at a quicker speed, which is especially beneficial for young children and patients with insufficient compliance. Previous studies have been applied to assess morphological alterations with aging (12,13), record characteristics of healthy subjects, and evaluate the conditions of impairment or malformation such as the cleft palate (14-17).
Thus far, a series of research mainly studied the 3D photogrammetry concerning the maxillofacial morphology. In contrast, few studies have focused on the 3D evaluation of the surface in the periorbital region. Gibelli et al. (18) captured face images of 14 volunteers using both stereophotogrammetry and a laser scanner. They then verified the concordance between 14 linear distances, 12 angles, as well as facial area and volume. They located the periorbital landmark of lateral canthus and measured the palpebral fissure’s inclination versus the horizontal plane. Gibelli et al. (14) conducted another research to validate a portable stereophotogrammetric device versus a static one to verify its applicability to 3D facial analysis. They acquired 3D facial photographs of 40 volunteers using portable and static devices. The medial canthus and lateral canthus were set as periorbital landmarks.
Regarding research focusing on the periorbital region, Li et al. (19) performed a cross-sectional study using a standardized 2D photogrammetry obtained from 162 Chinese young adults aged 20 to 30. They defined several landmarks, including palpebral superius and palpebral inferius (the highest and lowest points of the free margin of upper eyelid), medial canthus and lateral canthus (the soft tissue point at the inner and outer commissure of the palpebral fissure), as well as upper lid crease superius (the highest point of double lid crease). Subsequently, a series of linear and angular anthropometric parameters between these landmarks were measured, i.e., palpebral fissure length and height, inter- and outer-canthal width, crease height, angles of the medial canthus and lateral canthus, as well as the axis of the palpebral fissure. They then calculated the palpebral fissure index, canthal index, and angular index. Jayaratne et al. (20) conducted the first study creating a database of 3D periorbital anthropometric norms applying 3D stereophotogrammetry. They adopted a 3dMDface system to acquire the craniofacial images of 103 Chinese subjects aged between 18 and 35. They then measured linear distances (intercanthal width, binocular width, eye fissure height, and eye fissure length) between several anthropometric landmarks (palpebrale superius, palpebrale inferius, lateral canthus, and medial canthus) identified on these digital 3D images. Jodeh et al. (21) proposed a new method to measure normative facial projection relative to the pupil. They adopted the landmarks of bilateral pupils, supra- and infra-orbital rims, lateral orbital rims, lateral and medial canthi, as well as midline nasal radix.
However, no research in 3D periorbital anthropometry has been performed in surgery planning and treatment outcome evaluation. That is partially due to the lack of detailed and standardized 3D periorbital landmarks as well as normative anthropometric parameters database in the periorbital region regarding linear distance, angle, curvature, among others. With standardized parameters, surgeons may compare different results in various studies and precisely follow up the pre- and postoperative 3D morphological alterations of the surface in the periorbital region.
Guo et al. (22,23) proposed a novel standardized 3D anthropometric landmarks localization protocol for the periocular (or periorbital) region, which is beneficial for standardizing 3D periorbital anthropometry and minimizing the localization errors among various studies. The subjects were seated in front of a 3D camera. They opened their eyes and gazed forward into a mirror in the middle of the 3D camera. After taking a 3D photograph of each subject, an experienced researcher performed this protocol with the aid of coordinate axes in software. At the beginning of this protocol, five landmarks were set as prime points on each 3D periorbital model. They are the pupillary center (Pc), the intersection point of the medial or lateral limbus and the horizontal line passing through the pupillary center (Lm or Ll), medial canthus (En), and lateral canthus (Ex). The En was identified as the vertex of the inner canthal angle, and the Ex was localized at the lateral commissure of the superior and inferior eyelash lines. These five landmarks were proved to be simple, reliable, and easily identifiable. Subsequently, a series of landmarks were placed vertically to one of these five landmarks (Figure 1 and Table 1).
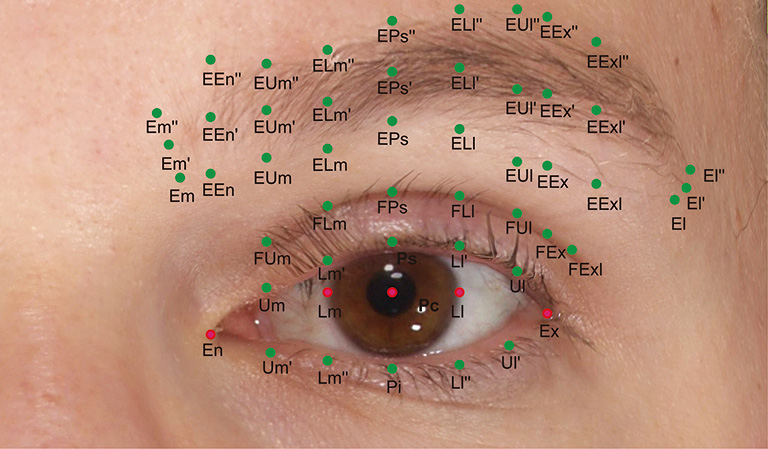
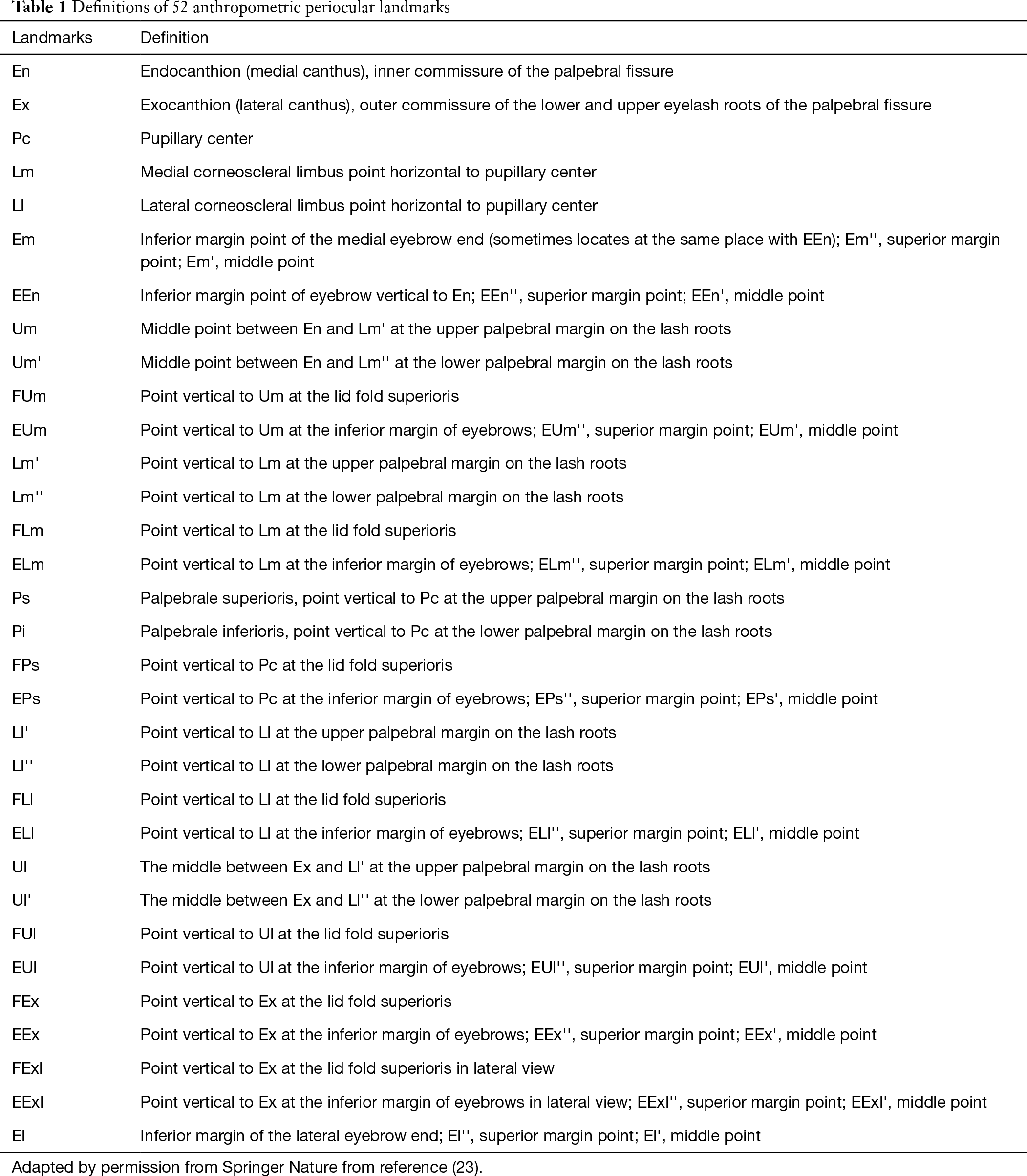
Furthermore, they defined the periorbital parameters between these landmarks as three categories, i.e., palpebral fissure-related, upper lid fold-related, and brow-related parameters (Table 2) (22,23). Besides, they established a 3D periorbital morphology database for young Caucasians and analyzed the differences between sexes. They found a statistically significant difference in 63% of the linear distances, curvatures, angles, and indices between sexes. A correlation between aesthetic assessment and several periorbital parameters was also shown in this study (22). Specifically, a positive association with the aesthetic assessment was found in palpebral fissure height and eyebrow-palpebral margin distance (medial limbus); and a negative in canthal tilt, eyebrow-medial canthus distance, and eyebrow length.
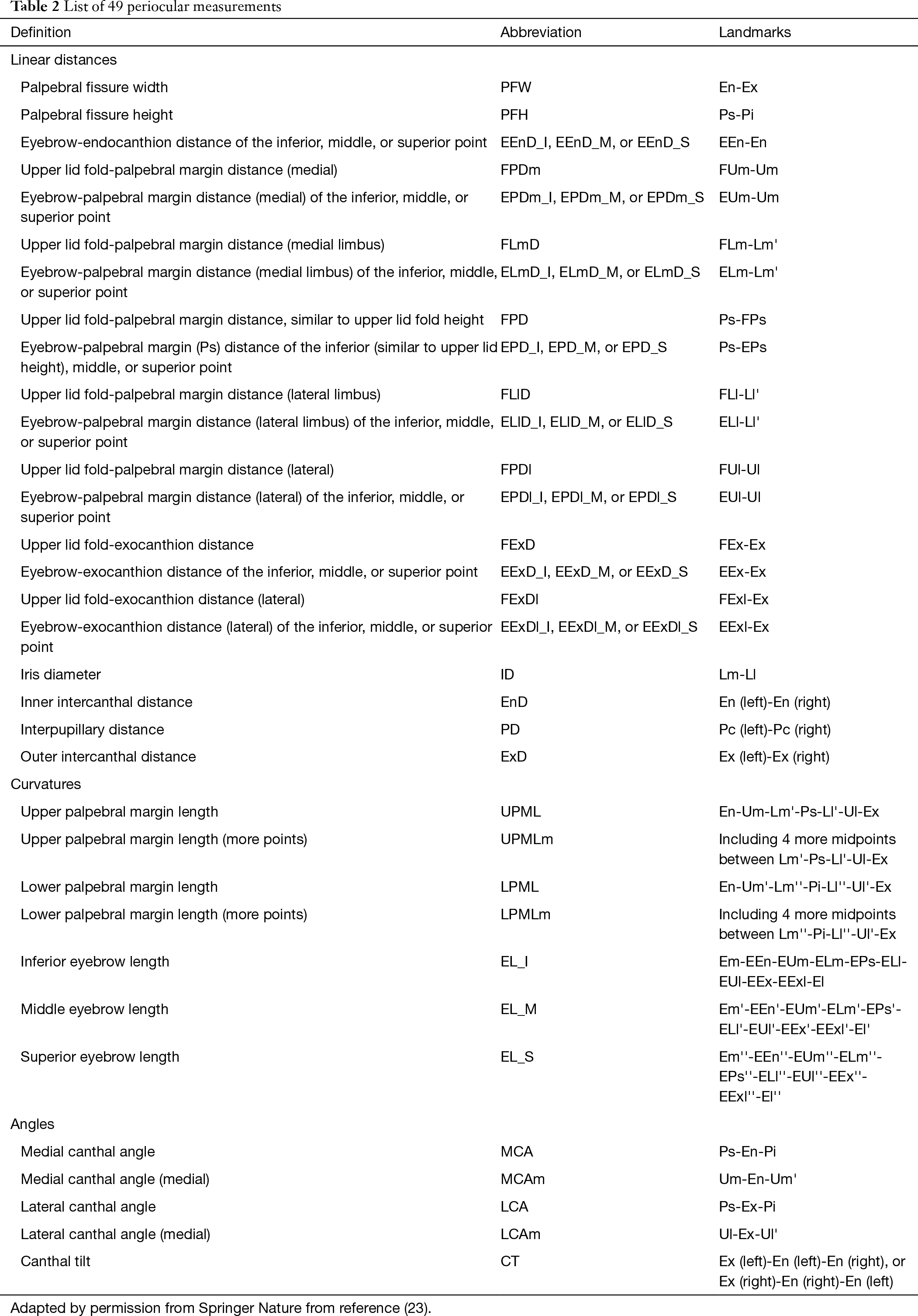
In addition, attention has also been paid on the assessment of eyebrow height due to the close anatomic correlation between the eyebrow and the eyelid as well as the palpebral fissure. Various approaches have been proposed to describe the eyebrows’ position across different ages, genders, and ethnicities (24-26). Guo et at. (22,23) measured the distances between the eyebrow (at inferior, middle, and superior margin points, respectively) and the upper palpebral margin (at landmarks corresponding to the above-mentioned prime points, i.e., the medial canthus, lateral canthus, pupillary center, medial limbus, and the lateral limbus). Kokubo et al. (27) adopted three landmarks, i.e., the medial canthus, the pupillary center, and the lateral canthus, to assess the eyebrow height on 2D photographs. They drew a horizontal plane between the right and left medial canthi. The pupillary center and lateral canthus were reflected on this plane. Eyebrow height was deemed the distance between these points on the plane and the eyebrow’s superior margin. Besides, other studies involved the distance between the pupillary center and the lower eyebrow margin (28), the distance between the pupillary light reflex and the midpoint of the eyebrow (29), among others.
Before extensively spreading in clinical practice, all technologies should be validated entirely for measurement errors (30). Ulijaszek et al. (31) reviewed various anthropometric measurement error types and critically evaluated the methods of estimating measurement error. Although various terms have been reported to evaluate anthropometric measurement error in previous studies, two categories of possible measurement error are predominantly described as following: (I) the degree to which repeated measures obtain the same value; and (II) the close degree for a measurement to its “true” value.
Of the first category, reliability, unreliability, precision, imprecision, and reproducibility are the most commonly used terminology in addition to undependability. The studies that evaluated the reliability of 3D photogrammetry commonly meant to figure out the degree of unreliability. Precision and imprecision have been the most commonly used evaluation index for anthropometric measurement errors (14,18,23,32-39). Imprecision is the variance of repeated measurements, e.g., intra-observer measurement error (i.e., within-observer error) and inter-observer measurement error (i.e., between-observer error). Ulijaszek et al. (31) described the calculating procedures of technical error of measurement (TEM), relative TEM (rTEM), coefficient of reliability (R), and intraclass correlation coefficient (ICC) in detail to estimate imprecision. Guo et al. (23,39) evaluated the intra- and inter-observer reliability as well as intra-method reliability of their standardized periorbital 3D photogrammetry technique. They calculated TEM, rTEM, total TEM, mean absolute difference (MAD), relative error measurement (REM), and ICC. The calculation procedure and acceptable levels of measurement error have been proposed as follows:
Andrade et al. (40) analyzed the repeatability of a stereophotogrammetry system for evaluating facial morphology. They marked 11 maxillofacial reference landmarks on each subject’s face, including the glabella, nasion, pronasale, columella, subnasale, labiale superius, labiale inferius, labiale sublabiale, pogonium, menton, tragus. Nine angular measurements and two linear measurements were obtained. They calculated the MAD, REM, TEM, ICC, and conducted a Bland-Altman analysis for repeatability analysis. They found that the nasolabial and mentolabial angles were larger than 2° (clinical limit) in TEM. All measurements were between good and excellent consistency for REM, except for the maxillofacial angle (moderate). The nasolabial, mentolabial, facial convexity, full facial convexity, maxillofacial, and nasofrontal angles were deemed excellent for ICC. In the end, they concluded that the stereophotogrammetry was repeatable and may give accurate measures within their references.
As for the periorbital region, Jodeh et al. (21) found less than 0.5 mm of standard deviations for repeat measures of bilateral pupils’ landmarks, supra- and infra-orbital rims, lateral orbital rims, lateral and medial canthi, as well as midline nasal radix. Intra-rater reliability was high for all these landmarks (ICC: 0.93 to 0.99). Inter-rater reliability was excellent for all landmarks except for the lateral canthion. They concluded that their technique might apply to evaluate surgery outcomes and growth alterations on the facial project. Guo et al. (23) identified 52 periorbital landmarks and then analyzed the intra-rater, inter-rater, and intra-method reliability of 49 linear, curvilinear, as well as angular measurements. For intra-rater 1 and intra-rater 2 reliability, they found highly reliable results for MAD (0.59 and 0.68 unit), REM (2.66% and 3.08%), TEM (0.59 and 0.66 unit), rTEM (2.71% and 2.96%), and ICC (0.98). For inter-rater reliability, the results showed 0.94 unit in MAD, 4.06% in REM, 0.89 unit in TEM, 3.94% in rTEM, and 0.97 in ICC. Regarding intra-method reliability, the MAD was 0.98 unit, REM 4.66%, TEM 0.96 unit, rTEM 4.64%, and ICC 0.96. They concluded that this stereophotogrammetry and the landmark localization procedure were highly reliable for periorbital anthropometry.
Besides, they also evaluated the reliability of 22 periorbital measurements obtained by direct anthropometry, 2D photogrammetry, or 3D stereophotogrammetry (39). They then compared the reliability levels of each measurement among these three techniques. The results showed that, for direct, 2D, and 3D techniques, overall intra-rater ICC was 0.88, 0.99, and 0.98, respectively; overall intra-rater MAD was 0.84 mm, 0.26 units, and 0.35 units, respectively; overall intra-rater TEM was 0.85 mm, 0.25, and 0.32 units, respectively; overall intra-rater REM was 6.46%, 1.69%, and 1.67%, respectively; overall intra-rater rTEM was 6.25%, 1.62%, and 2.12%, respectively. Furthermore, for 2D and 3D techniques, overall inter-rater ICC was 0.97 and 0.92; overall inter-rater MAD was 0.36 unit and 0.67 unit; overall inter-rater TEM was 0.36 unit and 0.65 unit; overall inter-rater REM was 2.74% and 5.11%; overall inter-rater rTEM was 2.78% and 5.12%. Therefore, they concluded that the stereophotogrammetry and their landmark identification protocol might be applied for 2D and 3D periorbital measurements due to the very good reliability.
Of the second category, bias, validity, accuracy, and inaccuracy are the terms commonly used. Accuracy is the degree to which the “true” value of a measurement is given. Validity involved the value measured, which is conceptually approximate to accuracy. The measurement obtained by a gold standard tool is considered the “true” value of a characteristic in practice. Inaccuracy is a systematic bias that may occur due to the error from either equipment or measurement technique.
It is thought that complex equipment may yield a more significant inaccuracy of measurement than a simple one. Therefore, Ulijaszek and Kerr (31) believed that a simple tape measure is likely to give more accurate results than a sophisticated instrument involving sliding scales, e.g., anthropometers and stadiometers, while assessing the status of nutrition by measuring skinfolds. The calipers may compress the skin, causing surface deformation and landmarks displacement with corresponding soft tissue measurement differences.
Although direct anthropometry using sliding and spreading calipers may be inaccurate, it remains the gold standard for anthropometry in craniomaxillofacial surgery due to its simple, operable, and affordable characteristics. Therefore, various novel anthropometry techniques are commonly compared with the direct technique to evaluate their accuracy. Dindaro?lu et al. (34) compared 3D stereophotogrammetry with the direct and 2D photogrammetry techniques to evaluate 3D stereophotogrammetry accuracy in six profiles and four frontal parameters. They also examined the reliability coefficient between methods. Their results showed the highest MAD of 0.30 mm between direct and 2D techniques, 0.21 mm between direct and 3D techniques, and 0.5 mm between 2D and 3D techniques. As for reliability, the nasal tip protrusion was found the lowest agreement ICC value of 0.965 between 2D and 3D techniques. Weinberg (41) compared a set of 24 standard soft-tissue craniofacial linear distances between two datasets, i.e., the 3D facial norms obtained by stereophotogrammetry (n=2,454) and the Farkas craniofacial norms gained by direct anthropometry (n=2,326). To evaluate both data sets’ discrepancy, they calculated standardized effect sizes (Cohen d) for all measurements to assess its overall direction and magnitude. The mean d value is positively correlated with the discrepancy across datasets, e.g., the higher the mean d value is, the greater is the discrepancy. They found a more significant discrepancy in measurements involving the landmarks of tragion (the point anterior to the external auditory canal at the upper margin of the tragus) and nasion (the intersection of the midline and the frontonasal suture). Besides, the width of nasolabial structures, the lip involving vermilion, and the palpebral fissure length was also found more considerable differences between the two datasets. Therefore, they concluded that there were considerable discrepancies between both norms obtained by 3D stereophotogrammetry or direct anthropometry.
Furthermore, previously validated stationary 3D surface imaging systems have been applied to validate recently invented low-cost and portable 3D imaging systems due to high accuracy and reliability. Camison et al. (32) took 3D facial photographs of 26 adult individuals with the handheld Vectra H1 and a previously validated 3D imaging system 3dMDface system. They then evaluated the error magnitude statistics of 136 linear facial distances and global root mean square (RMS) error of 26 surface -to surface comparisons. The results showed highly comparable measurements in these distances across both cameras (mean TEM =0.84 mm, ranging between 0.19 and 1.54 mm). The mean RMS was 0.43 mm (ranging between 0.33 and 0.59 mm). Therefore, they concluded that 3D facial surface photographs captured with the portable system were adequately accurate for most clinical applications.
Besides, it is a challenge to perform direct anthropometry in the periorbital region. Involuntary blinking and soft tissue deformation increase the measurement errors, which is especially crucial for a small size. Furthermore, physical contact may injure the eyes’ delicate structures, increase the operating time, and depend more on patient cooperation. Therefore, 3D anthropometry may be a future trend and become the gold standard for periorbital anthropometry in the future. In Weinberg’s study (41), the author evaluated three periorbital parameters, i.e., inner canthal width, outer canthal width, and palpebral fissure length. A more significant discrepancy between 3D and direct anthropometric datasets was shown in palpebral fissure length. They attributed the significant discrepancy to inadequate open and relaxation of the eyes due to direct anthropometry’s physical contact nature. Hyer et al. (42) conducted a cross-sectional study to assess the accuracy and inter-observer reliability of 3D stereophotogrammetry for volumetric measurements in the periorbital region. They also proposed a protocol for acquiring volumetric data using 3D systems in this region. Exactly, they took 3D photographs of 58 adult subjects on two independent occasions and then performed 40 different measurements of volume for each side. Subsequently, they calculated the mean periorbital volume alterations between different methods, i.e., two registration methods (facial landmarks tool and surface area paint tool), open or closed eyes, separate or integrated upper and lower eyelids, lower eyelid with or without mid-face (tear trough and palpebromalar groove). A significant difference was indicated between different methods of measurement. The most accurate method showed the mean alteration in volume of 0.11±0.13 mL. The highest agreement between two independent observers was 0.63 for ICC. As a conclusion, they claimed that the 3D imaging system is accurate and suitable for assessing periorbital volumetric alteration in clinical practice, with good inter-observer repeatability.
In summary, 3D anthropometry has become increasingly popular in clinical practice to date. The current studies have proposed detailed and standardized protocols for three-dimensionally assessing linear, curvilinear, angular, as well as volumetric measurements, and verified its high reliability in the periorbital region (even higher than caliper-derived direct measurements) (22,23,39,42). In the future, reliable and accurate 3D imaging techniques, as well as standardized analyzing protocols, may find applications in following up morphological growth, preoperatively diagnosing and assessing patient periorbital conditions, planning surgical procedures, postoperatively evaluating treatment outcomes of a specific procedure, and comparing the differences in surgical results between various procedures, studies, as well as populations.