Background: To study the application of management tools such as Plan-Do-Check-Action (PDCA) cycle and fishbone diagram in optimizing surgical procedures to improve the satisfaction of doctor-nurse-patient.
Methods: The fundus surgery nursing team of our hospital began to implement the PDCA cycle management mode to optimize the surgical procedure from July 2017, set up a project activity improvement team, unified the surgical labeling processing plan, and made the fundus surgery procedure, and established the preoperative health education for surgical patients, and standardized the training content of post-rotating doctors and interns.
Results: The satisfaction degree to surgical procedure after implementation of doctors and nurses was higher than that before implementation.
Conclusions: Using PDCA cycle and fishbone diagram analysis tools to manage the surgical procedure optimization can better integrate doctor-nurse medical care, improve the efficiency and accuracy of the surgical procedure delivery and operation, and optimize the satisfaction of the three parties of doctor-nurse-patient.
Satisfaction survey is an important basis for building a harmonious doctor-patient relationship. It is an important indicator to measure the quality of hospital services. In order to further strengthen hospital management and continuously improve the quality of medical services, we conducted it as an important evaluation indicator for the implementation of refined management in our hospital. The Plan-Do-Check-Action (PDCA) cycle, also known as the Deming Cycle, is an enterprise management method summarized by Dr. Deming, a US management scholar. The cycle activities were abbreviation of Plan, Do, Check and Action. The PDCA cycle theory was first applied for enterprise management and recognized by the management community as one of the effective management methods. It has penetrated various fields and has been widely used in the medical industry and has achieved good results (1). In 2017, our fundus surgery venter took the lead in conducting full-day surgery. In order to improve the satisfaction of the ward after the development of the day ward, we tried to apply the PDCA cycle management method to improve the satisfaction of medical staff and patients in the ward and achieve good results. It is reported as follows.
Our hospital fundus surgery project activity improvement team has a total of 7 nursing staff, aged 28–45 years, with the length of service 4–28 years, including 1 nurse in charge and 6 senior nurses. There are 1 team leader, 1 deputy team leader and 5 team members.
The PDCA cycle (2) is a comprehensive and important quality management tool for fundus surgery in our hospital. In recent years, the optimization of the surgical procedure has been improved in stages, and the effect is remarkable. All studies adhered to the tenets of the Declaration of Helsinki. And this study is also a retrospective analysis of the defects in the surgical process of fundus surgeons and nurses in our hospital in 2017, so which does not involve ethical issues.
Fishbone diagram analysis: a method of mapping analysis that reveals the cause of the problem through a clear fishbone frame diagram. During the drawing process, the causes of the problem will appear one by one. By using this method, a clearer context can be obtained, and the essence of things can be grasped.
In 2017, we used PDCA for one-year optimization and improvement for the defects in the surgical procedures including picking up patients of the fundus surgery doctors and nurses in our hospital. Firstly, the fishbone diagram analysis method was used to find and analyze the causes of defects from three aspects of doctor-nurse-patient, as shown in the following Figure 1:
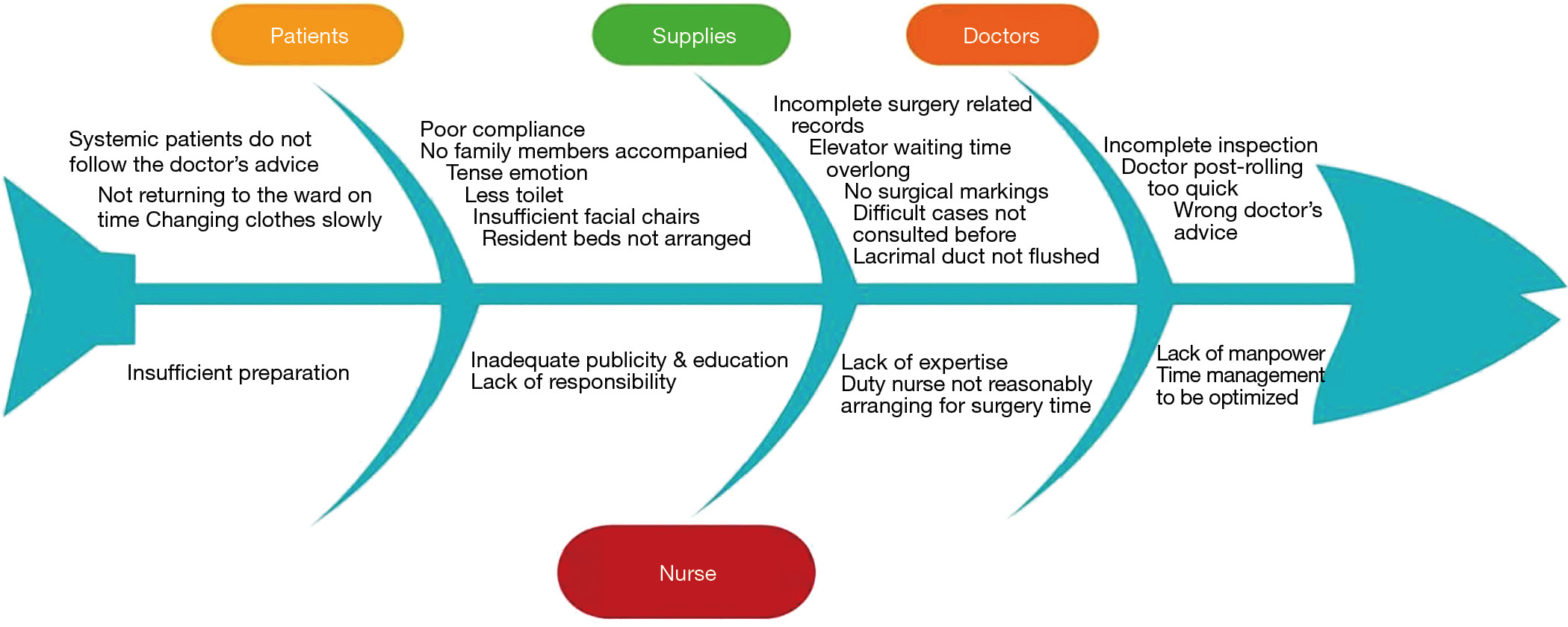
Patients and staffs of wards and operating room failed to form effective communication, as well as the imperfect preoperative visits, and unclear management procedures were the key factors affecting the efficiency of the surgical procedure (3).
(I) There was mistake in doctors’ advices, the operation related records and the informed consent form were not perfect, the doctors were not familiar with the operation of giving advices; (II) the surgical mark was not done, the marking of operation in the ward was not clear; (III) the content of patients’ preoperative health education was vague and random, without making unified specifications. And the inspection data was not complete without careful check.
(I) Nurses did not pay attention to the patients’ health education; (II) patients did not know what services they would receive because services items were not disclosed; (III) busy work and insufficient human resources; (IV) elevator waiting time overlong, lack of adequate resource allocation.
According to the reasons for each problem in the fishbone diagram, the project improvement team developed improvement methods one by one: (I) strengthening the training course for post-rotating doctors and interns; (II) unifying surgical labels for the ward; enhancing communication with doctors, and let them be aware of the importance of surgical signs; (III) strictly checking the prehospitalization and preoperative data, inform the doctor of the lack of inspection results and make a timely replenishment.
The surgical contraindications are as follow: ECG abnormalities such as myocardial ischemia, old myocardial infarction, atrial fibrillation, pre-excitation syndrome, frequent ventricular premature beats, acute myocardial infarction, ventricular tachycardia, cardiac tachycardia with heart rate more than 180 times or bradycardia less than 40 times. Patients with fasting blood glucose <3.9 or ≥10 mmol/L or postprandial blood glucose ≥14 mmol/L, systolic blood pressure ≥180 mmHg or diastolic blood pressure ≥100 mmHg should be notified to the corresponding bedside clinician for extended surgery.
We used different color modules to distinguish patients: patients undergoing surgery, patients to be sent, and those waiting for surgery, ongoing surgery, resuscitation status, surgery completed, returning to ward, surgery cancelled, discharged patients and so on. By this measure, unnecessary waiting time can be saved, and the corresponding patients could be found at the first time, thereby the surgical procedure would be completed more quickly.
Doctors and nurses formed a relatively fixed team; the ward rounds were fulfilled by doctors and nurses jointly, the nurses’ work turned from passive to active; thus, medical staff could master more professional knowledge, improve their operation level, provide better service for patients and reduce doctor-patient contradiction due to poor communication, meanwhile improve the satisfaction of doctors and patients on nursing work.
Early post: 7:00 AM: the number of operators was decided according to how many surgery operations undergoing: 1 person (≤3 surgery operations); 2 persons (4–5 operations); 3 persons (≥6 operations); the post of 7:30 AM: adding a person to support time post of 7:00 AM. The surgical posts were divided into eye wash, treatment and check posts.
In order to achieve specific job responsibilities, avoid work duplication, reduce errors, and improve work efficiency. We divided the admission registration cards into three sections: doctor, nurse and surgery operation duties. Each section clarified the duties of different positions. The doctors were responsible for reviewing the physical examination results of the whole body, the results of the intraocular lens measurement, reviewing the old medical records, and signing the informed consent form of surgery, printing case-related documents, and measuring the patients’ intraocular pressure; the nurses were responsible for asking about the patients’ systemic medical history, allergic history, preoperative use of anti-inflammatory eye drops, anesthesia ways (such as general anesthesia, need to explain the patients’ fasting and water deprivation time), health education and measurement of height and weight; Surgical post was responsible for preoperative intravenous infusion, implement of intramuscular injection or oral administration, perform mydriasis for patients requiring preoperative mydriasis according to doctor’s advice, preoperative fingertip blood glucose measurement for diabetic patients. When completing the corresponding duties, you need to type √ in the small box behind the corresponding responsibilities items, so that medical staff in different positions could determine whether the patient had prepared for the preoperative work.
We strengthened the pre-job training of the post-rotating doctors and advanced training physicians, standardize the doctor’s advice template, unify the treatment plan of the departmental surgical marks, establish a group for medical work communication, and make the doctors’ bed and the operation schedules.
In the peak period of the surgery process, personnel diversion was used to improve efficiency: the personnel were divided into treatment room and ward classes. The former flushed the conjunctival sac in the treatment room; the latter was responsible for measuring the patients’ vital signs and performing intravenous infusion in the ward.
The original 4-person-position was adjusted to 6-person-position, and make the originally idle space effectively utilized to speed up the surgical pick-up process.
We developed preoperative health instruction manual and audio for patients with fundus surgery, including diet, exercise, medication, related precautions, etc.; strengthened evaluation, education, and effect confirmation of surgical patients. Then we made scrolling broadcast the above contents through the recorder.
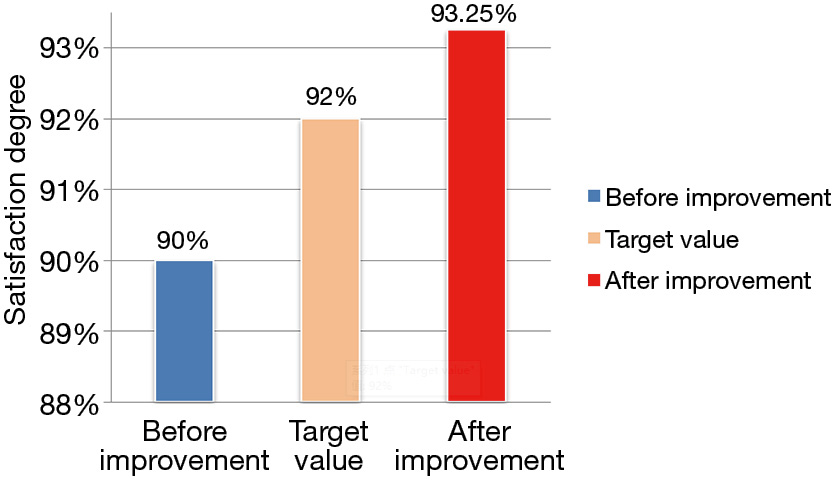
We regularly monitored the improvement process every month, recorded the improvement effect, evaluates the completion quality, checked the improvement schedule, and adjusted the work progress. We also regularly assessed the patients’ satisfaction degree to doctors and nurses. The satisfaction degree after improvement (93.25%) was significantly higher than that before the improvement (90%), as shown in Figure 2.
We regularly summarized the improvement of the picking up surgery work and consolidated it as a standard of operation. The retrospective analysis was carried out continuously during the work, and we continued to enter the PDCA cycle by discovering the deficiencies and problems in the work process, so as to constantly improve the quality of work (4).
The management of picking up patients in the ward is an indispensable part of the whole surgical procedure. The belated or wrong picking up due to the mindlessness and irresponsibility of the doctors or nurses may result in the operation being unable to proceed smoothly. In order to avoid the recurrence of this situation, it is necessary to use a reasonable method to optimize the current surgical procedure.
The use of PDCA cycle is to maintain the nursing care system and to carry out uninterrupted and long-term care work. This practice can help the nurses to find out the risks in the nursing process in time and systematically analyze the causes to find out the best solution. And try our best to avoid risks and continuously improve the quality of care (5).
The implementation of standardized management helps to enhance the spirit of teamwork, promotes ward nurses to provide continuous care for patients, strengthens effective communication between them, and avoids shirking responsibility on safety issues, thereby improving patients’ safety. Unnecessary disputes between doctors and patients are reduced and the active service awareness of nursing staff has been increased (6).
Through the use of fishbone diagram analysis, we clearly saw a series of problems and shortcomings in the picking up process of surgery for patients in the fundus surgery in our hospital, and then entered the PDCA cycle to solve some of the problems. Through the optimization of this time, from the satisfaction degree to doctors and nurses, there has indeed been some improvement. However, one single PDCA cycle is not enough to solve all the problems. It is necessary to continuously draw the fishbone diagram again, and enter the new PDCA cycle once again, and continue to sum up the experiences, so that the patient flow in the fundus surgery of our hospital tends to improve.