Karl Golnik, MD, MEd (Figure 1) is a neuro-ophthalmologist at the University of Cincinnati Gardner Neuroscience Institute; a professor of ophthalmology at the Cincinnati Eye Institute and the University of Cincinnati; and professor of Ophthalmology at the University of Louisville.

Currently, he is director for education for the International Council of Ophthalmology (ICO), past-president and current Secretary for International Relations of the International Joint Commission on Allied Health Personnel in Ophthalmology, chair of the Pan-American Association of Ophthalmology’s Resident Education Committee. He has received numerous resident teaching awards and has more than 130 publications in the fields of neuro-ophthalmology and medical education.
Aside from neuro-ophthalmology, Dr. Golnik has a strong interest in medical education; in particular teaching doctors how to teach. Through the ICO, he volunteers 1 week per month traveling internationally and conducting meetings to teach residency program directors how to be more effective educators.
The University of Cincinnati established the Department of Ophthalmology and Otology in 1896. At that time the main teaching responsibility was of medical students. In the early 1920’s an eye, ears, nose & throat residency was established. Initially it was just 1 year in duration but by the late 1920’s had become 2 years. In 1932, a separate 2-year ophthalmology residency was established and in 1957 it became 3 years in duration. The resident complement has increased from 2 to 3 residents per year in 1967 and then from 3 to 4 residents per year in 2008. In 2018, an integrated internship year was started that includes 3 months of ophthalmology. During residency time is spent at the University Hospital, Cincinnati Children’s Hospital, the Veterans Hospital and the Cincinnati Eye Institute. Subspecialty fellowships are offered in oculoplastics, cornea-refractive, cornea, pediatric ophthalmology, retina-vitreous, ocular oncology and neuro-ophthalmology. The training program is overseen by our program director, Dr. Adam Kaufman, and program coordinator, Shari Kinnebrew.
In the USA, the resident selection process includes an application submitted through a central service. The application includes a personal statement, medical school grades, research experience, three letters of recommendation, national standardized examination scores, leadership experience, honors and achievements. Most applicants have very good grades, high scores and research experience in ophthalmology. Ophthalmology is very popular and the selection process is competitive. We have about 550 applicants for our four positions each year. Forty-eight of the applicants are invited for interviews which are very important to assess communication skills and are heavily weighted in our selection process.
The American Academy of Ophthalmology’s (AAO) Basic and Clinical Science (BCSC) text books serve as the basic “what to know” content for ours and most postgraduate ophthalmology residency programs in the USA. Of course, these are supplemented with monthly journal clubs where faculty choose the most important articles in the various subspecialties to keep training as up-to-date as possible. In addition, our weekly grand round presentations provide another venue to update residents and faculty on the latest ophthalmic developments in knowledge and surgical skill. Both residents and faculty participate as speakers at these grand rounds. BCSC content is taught in didactic conferences that occur primarily on Wednesday afternoons. During this time, no clinical activities are scheduled for the residents. There is a weekly rotation amongst the various didactic subspecialty teaching interventions. Other conferences include biweekly evening fluorescein angiography conference, quarterly evening cataract surgery conference and monthly Cincinnati Society of Ophthalmology evening meetings featuring many endowed lectureships with visiting professors from around the USA.
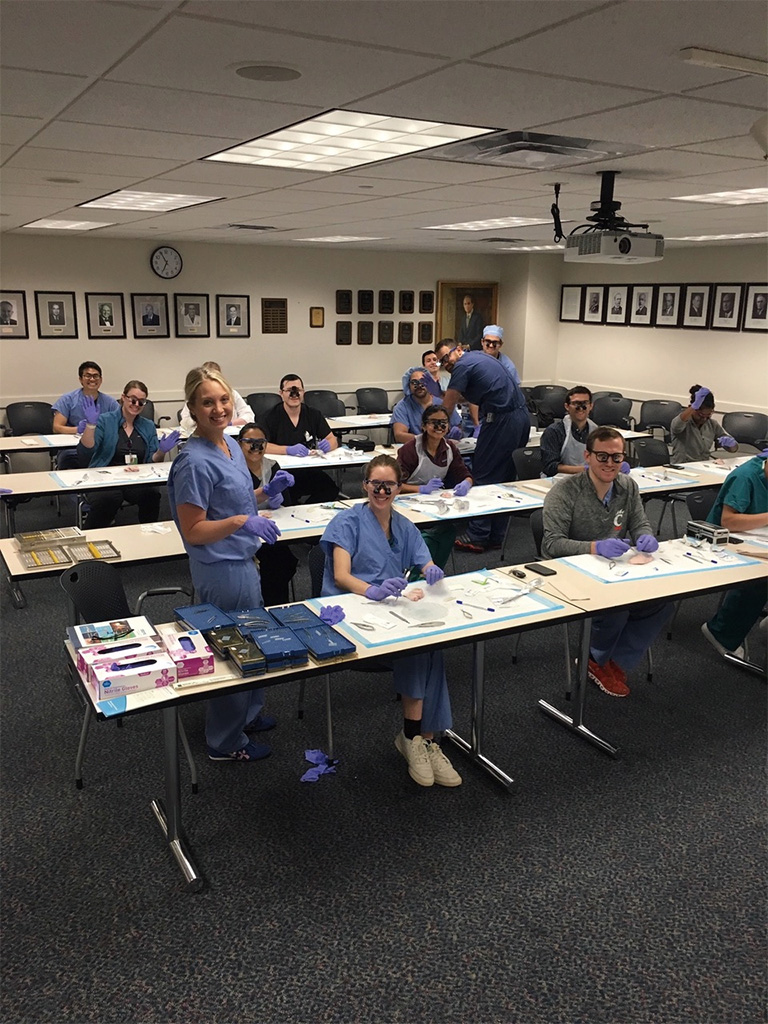
Each resident participates in exactly the same clinical rotations throughout the 3-year program. This guarantees an equivalent education for every resident. In most of the rotations, the resident is working one-on-one with relevant subspecialty faculty members. In our program, 55 faculty participate in these clinical teaching activities. The post-graduate year 1 (PGY1) is split between ophthalmology and several other areas. The resident spends 6 months on internal medicine, 3 months in ophthalmology and 1 month each of plastic surgery, emergency medicine and research. The PGY1 month of July is a structured orientation to ophthalmology and includes basic ophthalmology didactic conferences, surgical skill labs and clinical experience. The other 2 months are spent in the resident clinic and doing research. We have 4 residents per year and thus the year is split into four 3-month rotations. The PGY2 includes rotations at Cincinnati Children’s Hospital pediatric ophthalmology, Veterans Hospital (comprehensive ophthalmology), neuro-ophthalmology/refractive surgery and oculoplastics. PGY3 consists of glaucoma, cornea, retina and emergency ophthalmology/inpatient consults. The PGY4 has two rotations at the Veterans Hospital where the surgical volume is high, pediatric ophthalmology at Cincinnati Children’s Hospital Medical Center (CCHMC) and chief resident rotation at the resident’s clinic performing a variety of surgery. Residents start their surgical experience in PGY2 in the simulation center with wet-lab training (Figure 2), a virtual reality simulation curriculum (Figure 3) and gradually increase their surgical numbers as they progress through the PGY3 and PGY4 years. All surgical cases are logged in the national database and all minimum numbers are met for each surgical procedure as specified by our accrediting body the Accreditation Council for Graduate Medical Education (ACGME) (1).

Each resident is required to do at least one publishable research project during their residency. Preparation begins in the PGY1 year during a 1-month elective. A faculty mentor guides them through the process. The projects are presented at our annual Resident Research Day conference held toward the end of their training. In addition, each resident is required to participate in quality improvement projects addressing a variety of patient care issues such as clinic waiting time, electronic medical record issues, etc.
We use a variety of assessment methods to assess medical knowledge, clinical & surgical skill, professionalism and communication skills. The AAO provides a national standardized 250 multiple choice question test—the Ophthalmic Knowledge Assessment Program (OKAP) annually. Every resident in the USA takes this and overall raw score as well as percentile rank within PGY is reported. Sub-specialty scores are also given. The intent of this exam is to gauge knowledge and inform each resident as to their overall progress and their progress within individual subspecialties. We also conduct oral case-based exams on our neuro-ophthalmology and pediatric ophthalmology rotations. Clinical skills are evaluated informally on every rotation by the faculty member working directly with the resident. We also use the Ophthalmic Clinical Evaluation Exercise (OCEX) to provide more formal assessment and feedback (2). The OCEX is used primarily in PGY2 and PGY3. Surgical and procedural skills are also assessed directly by the faculty member involved. In addition, we use the Ophthalmic Surgical Competency Assessment Rubrics (OSCARs) from the ICO for a variety of surgical skills and procedures (3). The OSCARs are not used for every case, but rather intermittently and depending on numbers of cases and individual resident progression. Professionalism and communication skills are evaluated using the ICO 360-degree assessment tool (multisource feedback) on a quarterly basis (4). Every 3 months, the ACGME Milestones are completed using the results of the aforementioned assessment methods (5). This informs each resident as to their progress throughout the residency and informs the faculty of any problems as early as possible so remediation may be planned.
Within several months of successfully completing residency all residents take the American Board of Ophthalmology Written Qualifying Examination, a comprehensive, 5-hour, 250 multiple choice question test. One must pass this exam prior to taking the oral examination. The oral examination consists of a series of six 25-minute case-based mini-examinations. Once both tests are passed, the individual is considered to be “Board Certified”. Prior to 1992, board certification was for life but since then one must complete a maintenance of certification program every 10 years to assure continued competence (6).
All postgraduate medical training programs in the USA must be ACGME accredited. The process has changed in the past 5 years and now includes “continuous accreditation”. This process involves completion of an annual self-study to be completed by each program in addition to every 10-year face-to-face site visits (7). The ACGME also maintains the resident case log system. This process of accreditation protects the resident’s education, assures high quality, and standardizes training throughout the USA.