With the recent Coronavirus disease (COVID-19) pandemic we have experienced a sudden and dramatic change of our scheduled work in every field of medicine, including ophthalmology (1-3).
Our Medical Retina (MR) service is usually overbooked because of the increasing demand of intravitreal treatments for exudative maculopathy (4,5). However with the ongoing pandemic and the restrictive measures adopted by our Government to limit the spread of the COVID-19 outbreak, only urgent cases have been allowed to attend the clinic during the pandemic peak. Therefore, we had to swiftly reorganise and reschedule the planned activity of our Service. The electronic medical records (EMR), clinical notes and retinal imaging of patients booked in our MR service were reviewed in order to assess the eligibility of patients to attend the Clinic.
Approximately thirty patients per day were phoned with the aim to assess their visual condition. Among the patients scheduled for the intravitreal therapies nearly half of them reported stability of vision. Of the remaining half who reported a drop of visual acuity, approximately half of them refused to come to the hospital because of the risk of COVID-19 infection. All the patients attending the clinic for intravitreal therapies were called at least once in a month during the peak of the pandemic (February–April 2020).
A scoring system (Table 1) based on demographic, clinical characteristics, and adherence to treatment of patients was applied for those patients already booked for intravitreal treatment. The priority of treatment was given to the patients with the highest score.
| Characteristics | Point |
|---|---|
| Age | |
| <50 | 5 |
| 50–60 | 4 |
| 61–70 | 3 |
| 71–80 | 2 |
| 81–90 | 1 |
| >90 | 0 |
| Retinal disease | |
| mCNV | 4 |
| nAMD | 3 |
| CRVO | 2 |
| BRVO | 1 |
| DME | 0 |
| Eyes being treated | |
| One eye with low VA in the fellow eye | 2 |
| Both eyes | 1 |
| One eye with good VA in the fellow eye | 0 |
| Tx phase | |
| New onset | 4 |
| Loading dose | 2 |
| Maintenance | 1 |
| Adherence to therapy | |
| Unable to contact | 0 |
| Illness | 0 |
| 1st time renouncement | –1 |
| 2nd time renouncement | –2 |
BRVO, branch retinal vein occlusion; CRVO, central retinal vein occlusion; DME, diabetic macular edema; mCNV, myopic choroidal neovascularization; nAMD, neovascular age-related macular degeneration; Tx, Therapy; VA, visual acuity.
The score was computed by reviewing the retinal imaging and the clinical history on both EMR and clinical notes by two MR consultants (SE and MM).
In line with the recent guidelines and expert panel recommendations on anti-vascular endothelial growth factor (VEGF) treatment during COVID-19 pandemic (6,7), fixed dosing treatment was maintained for stable patients. For patients on treatment with a treat & extend regimen, the interval that provided a fluid-free macula was maintained.
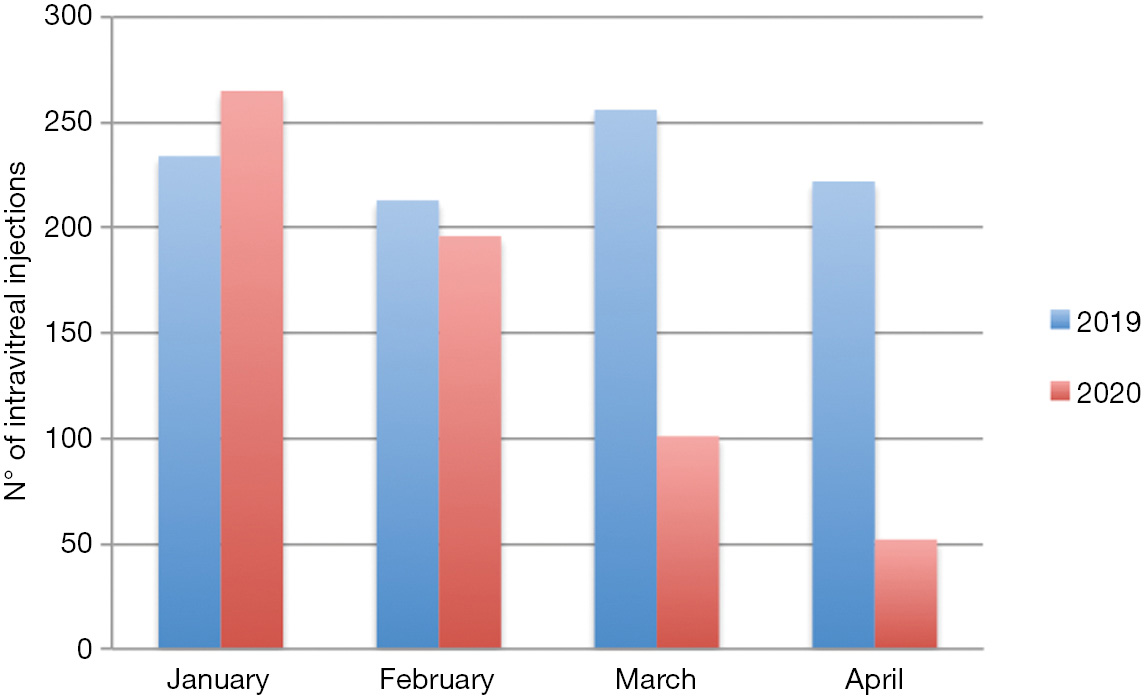
Our approach led to a remarkable decrease of the number of examinations and therapies delivered per day by our MR service, especially during the peak of the pandemic. Between February and April 2020, we performed approximately half of the injections performed in the same period the year before (Figure 1).
The decreased volume of visits and injections was aimed at avoiding the overcrowding of patients and carers in our clinic thus limiting contacts of patients, carers and health workers with possible sources of infection. However, this approach resulted in a certain delay of treatment in patients with a low score and therefore deemed to have lower priority than others.
Our approach has several limitations since we have not taken into account several factors such as the number of previous intravitreal injections, history of anti-VEGF switch and the lesions subtype. In our score we have given priority to young patients. Indeed, young age and myopic maculopathy, usually affecting patients younger than those with other exudative maculopathies, were given the highest points (Table 1). The reason of this choice is two-fold: blindness and low vision are increasing costs in our society and people in working age with eye disease could lead to early retirement, and social life limitations. Additionally, we sought to limit hospital visits in elderly people, who are at increased risk of complications and death following COVID-19 infection (8).
While we are aware of the limitations of our approach, COVID-19 pandemic was an unprecedented scenario that forced us to take tough decisions for a prompt reorganization of the clinic. We did not have the possibility to lean on proven strategies, since reliable guidelines came out after the pandemic peak in Italy (6,7,9).
In conclusion, our described approach, including the application of a scoring system for the patients eligible to the intravitreal therapy, helped us in the decision process about the priority of treatment among patients with exudative maculopathy during the COVID-19 pandemic peak in Italy. Follow-up of these patients is needed to clarify the effect of such approach in the long-term.