Abstract: RAF near point rule (RNPR) is a routinely used instrument in ophthalmology and optometry practice as well as for research purposes to measure the near point of convergence (NPC). The measurement of NPC is an important criterion for diagnosis and management of convergence insufficiency. The RNPR forms an important tool for ophthalmic clinicians however, only a very little is understood about it. This article tries to describe and review the designs, measurement techniques, merits and demerits of the RNPR and establish the need for its modification. It recommends that clinicians and researchers consider these findings while measuring NPC with the RNPR.
RAF near point rule (RNPR) also known as Royal Air Force (RAF) rule is a routinely employed instrument in ophthalmology and optometry practices to measure near point of convergence (NPC) and near point of accommodation (NPA). It is also used as a standard tool for research purpose and to provide therapeutic home-based orthoptic exercises (1,2).The assessment of NPC is an important part of a routine eye examination as it serves as the primary assessment for the diagnosis and management of convergence insufficiency (3-6). Convergence insufficiency is a non-strabismic binocular disorder and a common cause of asthenopic symptoms (7). Convergence insufficiency, affecting about 5% of the global population, may have a negative impact on the health-related quality of life, potentially causing difficulties with reading and associated near work (8,9).
The Convergence Insufficiency Treatment Trial (CITT) group included a receded NPC of 6 cm or more as an important criterion for diagnosis of convergence insufficiency along with an exophoria at near greater than distance by at least 4 prism diopters, and a decreased positive fusional vergence (PFV) at near (10). Most of the optometrists, however, consider NPC as the main factor in making a diagnosis of convergence insufficiency (11). Considering the clinical significance of measuring NPC, understanding the design, procedure, merits and demerits of RNPR can help us in properly measuring the NPC.
The RNPR was first mentioned in the literature by J. C. Neely in 1956. It stated that the RNPR was originally developed in the United Kingdom (UK) in the mid-1950s to assess the visual abilities of the individuals conscripted into the US military to carry out routine clerical responsibilities. The instrument was used to assess the visual functions like convergence and accommodation as well as to establish the correlation between distance and near visual acuity (12). After the introduction, its use has widely expanded and continues as a preferred ophthalmic tool. Apart from the UK and Ireland, it is popular in Asia, including Bhutan, India, and Nepal. The RNPR is marketed by Haag-Streit? as RAF binocular gauge.
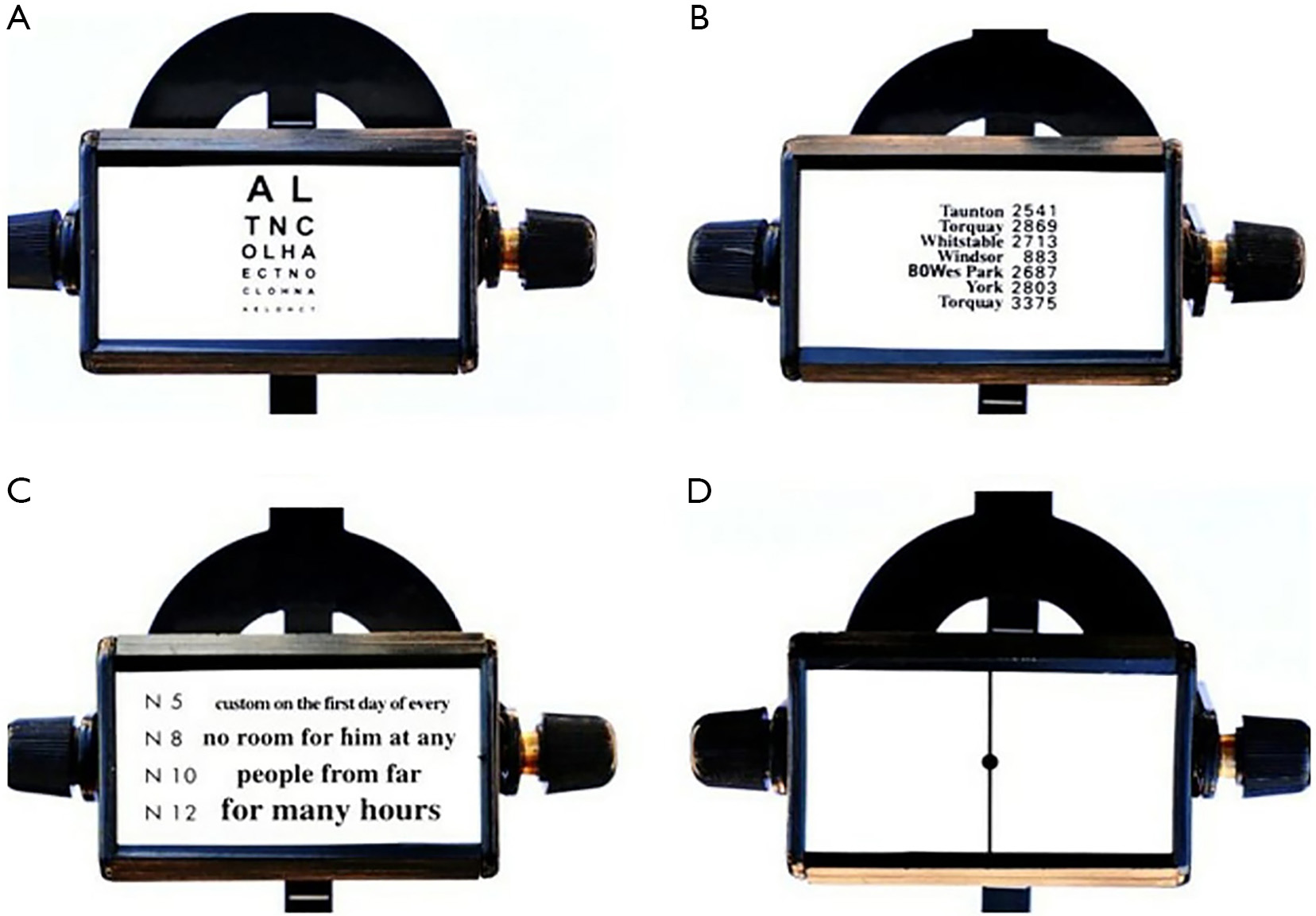
The RNPR consists of a rotating four-sided cubical drum held on a slider. The slider is attached to a square section metal rule. Each of the four sides has different accommodative targets with black prints on a white background which include:
Sides 1, 2 and 3 are used for measurement of NPA and side 4 is used for NPC.
The square rule which holds the drum is 50 cm long. This distance allows the measurement of NPC and NPA of presbyopes who prefer to read at 40 cm or more. Furthermore, it is also easier to determine the angle of 25 degrees from the eyes by a point at the end of a rule 23.3 cm in length (tan 250×50) held at 90 degrees to the end of the rule (12).
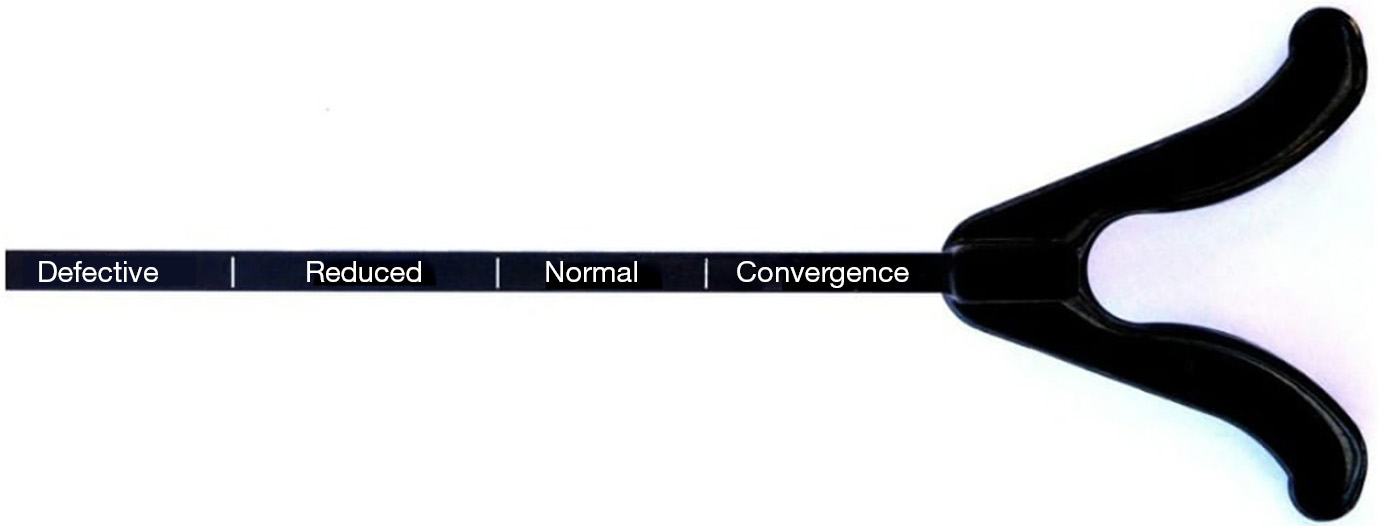
The four sides of the square rule are marked differently as; (I) a centimeter scale in 1 cm increment; (II) a corresponding equivalent dioptric scale; (III) expected age scale and; (IV) scale indicating the positions of normal and abnormal convergence.
The cheek rest of the RNPR (6 cm in length) is attached to one end of the rule. It is made of plastic and has a V-shaped notch in the center to fit the nose. The cheek rest allows the device to be comfortably placed on the subject’s cheek. The housing of the four-sided cubical drum is designed in such a way that the measurements can be read from the rearmost edge of the slider. The cheek rest results in the RNPR being positioned further from the plane of the eyes. This error in measurement is compensated by projecting the target forward by 6 cm (12).
RNPR measures both the subjective and objective NPC (15). Prerequisite for measuring NPC is the binocularity of a patient and a normal room illumination.
To measure the NPC, the dot on the line is the standard target. The examiner holds the ruler and gently places the cheek rest on the inferior orbital margin. NPC is most accurately measured by the RNPR in the depressed position of 45 degrees (16). The clinician asks the patient to focus on the black dot and slowly moves the towards the patient’s eyes at a constant and linear rate of about 1±2 cm per second (17).
The subjective break point is indicated when the patient either reports diplopia or until the slider is stopped by the cheek rest. The recovery is noted when the patient reports one target when the slide is slowly moved back. The objective values of break and recovery to binocularity are noted when the examiner notices that one or both eyes diverge from fixation and when both eyes regain triangulation on the target, respectively. All readings are measured to the nearest 0.5 cm.
Previous studies suggested that the test for NPC should be repeated to obtain a clinically useful information to diagnose convergence insufficiency, but there exists no agreement between the number of times the test should be repeated. Wick [1987] and Mohindra et al. [1980] recommended that the NPC should be repeated 4 to 5 times, while Scheiman et al. [2003] reported that the test should be repeated 10 times to yield significant clinical information (18-20). NPC should be measured 3 times at the beginning of the assessment and twice at the end to check for fatigue (16). Many patients manifest symptoms only after several minutes of near task.
The RNPR is considered the method of best practice for measuring accommodation and convergence, and forms protocol for eye testing, especially for the RAF and Civil Aviation Authority (21). Clinicians continue to use RNPR because it is easily available and new instruments are not introduced. Furthermore, because of its reproducibility, it is regularly used by researchers to measure convergence and accommodation (7,12,22,23).
There is also no effect of the proximity of the RNPR on the NPC. The study by Hung et al. [1996] reported that the relative proximal accommodation and proximal convergence induced by the use of RNPR were not clinically significant under simulated natural viewing environment (24). It is likely that these advantages make RNPR a preferred instrument.
The RNPR is designed such that the cheek rest cannot advance closer than 5.5 cm towards the patient’s face and allows the measurement the near point of convergence only up to 5.5 cm. However, many studies suggest that normative values for NPC are less than what could be measured by RNPR. Maples et al. [2007] demonstrated that to differentiate more and less symptomatic children the NPC break should be 5 cm or less (25). Several authors have assessed NPC between subjects with normal binocular vision and convergence insufficiency and suggested a clinical cutoff value of 5 and 7 cm for the NPC break and NPC recovery, respectively (5,20,26). Furthermore, recent studies have used NPC of six or less as a criterion for the diagnosis of convergence insufficiency (27-29). To overcome the drawback of the RNPR to accurately measure less than 5.5 cm, Paul Adler [2004] came up with a simple and low-cost modification to RNPR while maintaining its advantages (4).
The drum was extended with a Meccano? part on one side and a homemade plastic extension on the other side to bring the target closer than 5 cm.
RNPR is an accommodative target, and it can be less sensitive to evaluate NPC for the diagnosis of convergence insufficiency. The study by Pang et al. [2010] evaluated and compared NPC between an accommodative target (RNPR), a transilluminator (TR), and a TR with a red lens (RL) and found that the mean NPC break (with all targets) was less than 4.5 in the control group. It also showed that TR with a RL had higher sensitivity (100%) and specificity (88.9%) values compared to RNPR and proposed to use RL in suspected cases of convergence insufficiency (5). Thus, the credibility and reliability of RNPR become questionable.
It is assumed that the NPC measurement obtained with the RNPR is accurate. However, a few studies submitted that use of RNPR gives a more remote NPC compared to other methods. Adler et al. [2007] evaluated NPC with five different targets and found that when RNPR and penlight were used the NPC break point was more remote as compared to a pencil tip, fingertip, and N5 letters. They concluded that NPC determined with targets in free space would be more accurate as it correlates with the real world scenario (23). Similarly, Siderov et al. [2001] concluded that in a non-presbyopic population the RNPR gives a more remote NPC as compared to a pencil tip or a fingertip though the author considers it clinically insignificant (17).
The possible reason for receded NPC with RNPR is the pressure of the cheek rest on the face. The touch gives a proprioceptive feedback which might indicate that the target is closer than its actual distance and provides a stimulus to cease convergence and accommodation early, resulting in a more remote NPC (23).
Several studies have reported that the NPC break point would differ from the recovery point (17,20,21). Adler et al. [2007] reported that the average difference between NPC break and recovery is significantly decreased with targets mounted on the RNPR compared to the targets in free space. The relative difference is important in making the diagnosis of convergence insufficiency; the use of the RNPL rule makes it difficult to diagnose the borderline cases of convergence insufficiency (20). Furthermore, it was suggested that in the interpretation of results obtained by RNPR, one should use the NPC norms established using RNPR; similarly for targets used in free space (23).
There are also no recent studies to validate the use of RNPR and the design of the instrument has remained unchanged since its introduction in the mid-1950s. Nevertheless, clinicians still choose to use the RNPR. Though there is no evidence on why clinicians prefer to use RNPR, one possible reason could be the assumption that as long as cheek rest remains in contact with the subject’s face, the measured distances are correct. Moreover, it is expected that if targets are used in free space, the chances of errors are high if the subject or the clinician moves or is not steady. Another possible reason could be that most of the clinicians are not aware of the drawbacks of the RNPR.
NPC is the prime finding in the diagnosis of convergence insufficiency and RNPR is the traditionally employed instrument for the measurement is the NPC. Though the RNPR has a few advantages; there is no enough evidence to validate its use. More recent studies have highlighted the demerits of RNPR and favoured other methods of NPC measurement. There is a need to reassess and modify the design of RNPR to overcome its drawbacks and make RNPR more effective. In the meantime, it is recommended that clinicians and researchers consider the merits and demerits and follow the norms established with RNPR itself while measuring NPC with the RNPR.