Background: To report a new simplified surgical technique to manage small iris coloboma or traumatic iris defect.
Methods: A new surgical technique in which simplified pupilloplasty technique through only a clear corneal paracentesis to manage the iris coloboma or traumatic iris defect within the 120° range was designed. A retrospective revision of the medical records of patients treated with this technique between the years 2013 and 2016 was made. Six eyes of six patients with iris coloboma or traumatic iris defect treated with this new technique were included.
Results: All the operated eyes quickly recovered with central round pupil, negligible complications, inessential symptoms of photophobia and glare, and mild inflammation after a median follow-up time of 22 months (range: 6–34 months).
Conclusions: The simplified pupilloplasty technique presented here could be a good alternative for the management of small iris coloboma or traumatic iris defect.
Coloboma is a congenital malformation that ocular structures are incompletely formed due to failure of the embryonic optic fissure to fuse (1). It may include the eyelid, iris, lens, ciliary body, choroid, optic nerve, or retina, and cause mild to severe vision loss.
Iris coloboma can give rise to the so-called ‘‘keyhole’’ pupil or oval pupil clinically according to the effects on the iris pigment epithelium and stroma (2), which can be unilateral or bilateral. Although iris coloboma often occurs as a sporadic, isolated defect, it is frequently associated with clinically significant cataracts that develop at a young age. Another common cause of iris deficiency in clinical practice is trauma. Both cases may result in dysphotopsia, glare, reduced visual quality and monocular diplopia induced by the optic edge of the intraocular lens (2).
Once the patient has indicated that the identified iris defect causes them a functional complaint, a surgical intervention may be desired. An iris prosthesis may be the main viable alternative when the iris deficiency is massive (3-5). In addition, the choice of suture repair may be feasible when a defect is small and residual iris tissue is normal (6). However, management of the distorted and eccentric colobomatous pupil is still challenging.
Several surgical techniques to construct a more central and cosmetic pupil in these eyes have been developed. McCannel (7) first introduced the concept of suturing the iris within a contained anterior chamber by retrieving needles from small incisions in 1976. However, three wounds are required, even though this technique works best when the defect is reasonably peripheral, the iris tissue can be stretched, and the knot does not need to be overly tight. Alpar (8) first advocated the technique under Healon and made this technology easier to operate in 1985. In 1994, Siepser (9) described a slip-knot technique employing only two instead of three paracenteses, and decreased the damage of operation. Osher (10) described a modification of the Siepser slip-knot that allowed the knot to become locked, decreasing the chance of suture failure in 2005. All of these techniques can be technically challenging. We modified the pupilloplasty technique through only a clear corneal paracentesis to manage small iris coloboma or traumatic iris defect within the 120° range. Six eyes of five patients with iris coloboma or traumatic iris defect were treated with this new technique and achieved satisfactory results.
All cases that were underwent surgery between June 2013 and June 2016 for iris coloboma or traumatic iris defect, were selected from the hospital records. The Joint Shantou International Eye Center of Shantou University and The Chinese University of Hong Kong approved the study and ethic protocol. The study was conducted in accordance with the tenets of the Declaration of Helsinki. Inclusion criteria include patients who was diagnosed iris coloboma or traumatic iris defect (within 120° range) and received simplified pupilloplasty. Exclusion criteria include patients who received iris prosthesis surgery, or who performed suture repair and pupilloplasty using other technique, or those who failed to complete at least 6-month follow-up. The medical records were reviewed for demographic information, age at surgery, follow-up period, ocular and systemic associations, range of iris defect, details of surgical procedure, preoperative and postoperative visual acuity, pupil, photophobia, glare, monocular diplopia, amblyopia, and complications of surgery.
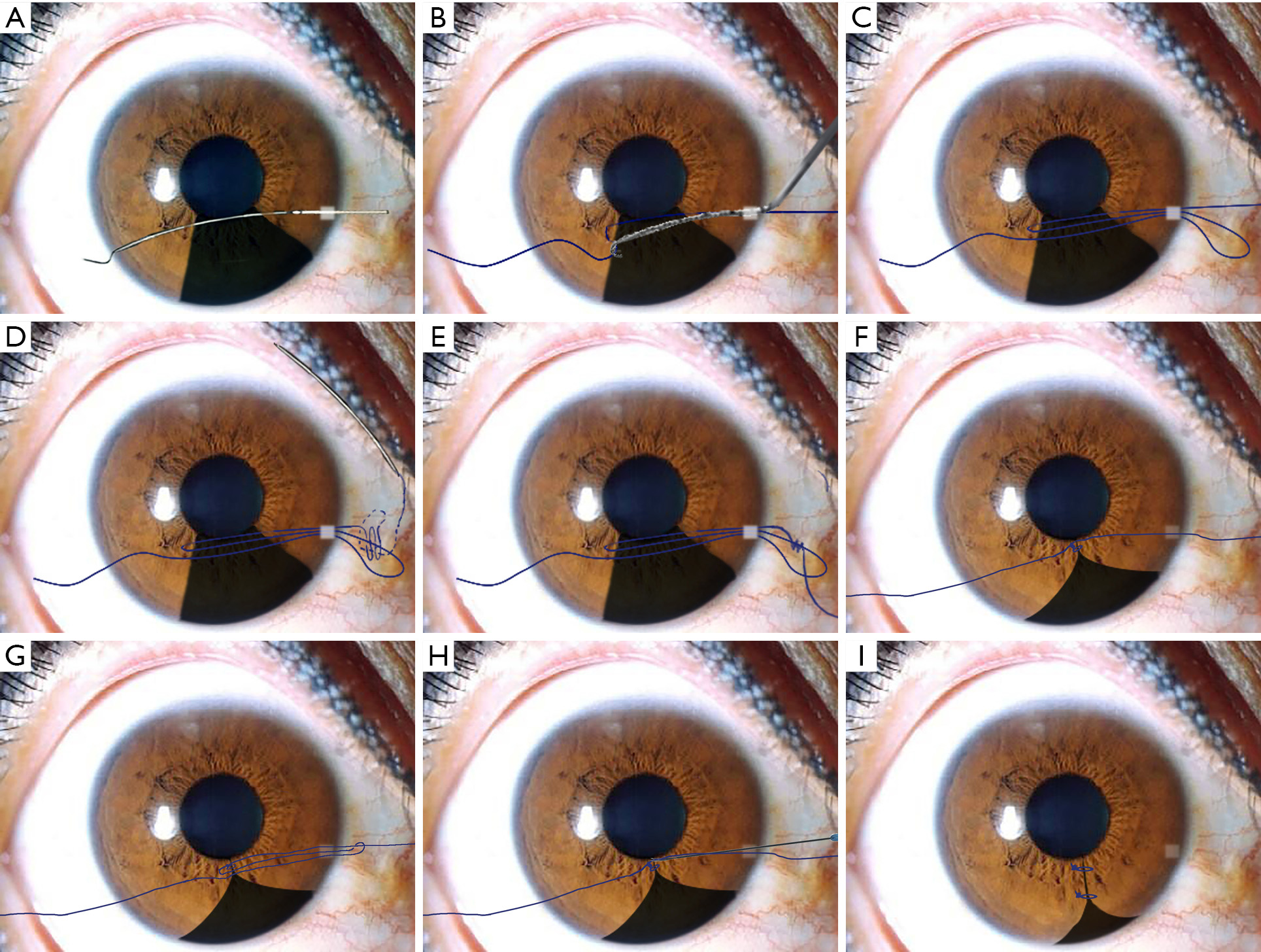
All surgeries were performed in the same hospital setting using a standard surgical technique. Briefly, a 1.0 mm clear corneal paracentesis was done in the vertical line of iris defect with 15 degrees knife, and viscoelastic agent was injected into the anterior chamber. A 10-0 polypropylene thread long needle, via the peripheral cornea of the opposite side of the peripheral corneal incision, through the defect iris edge, guided out through the clear corneal paracentesis with 30 G needle. A microhook was used to draw out the distal suture through the corneal stab incision. Tie a double knot sets using the long needle twist twice around the suture hooked out. Draw gently both the free end of the polypropylene suture, tighten the slipknot and cinch the two iris leaflets together. Hooked out the distal suture again, knotted in clockwise and tighten it. Repeat this procedure once again in counterclockwise. The free suture ends are cinched gently and complete the locking knot. At last, the ends of the suture are trimmed and removed (Figure 1).
After intraocular lens implantation, all operations were performed only through one peripheral corneal incision if combined with cataract phacoemulsification and intraocular lens implantation surgery.
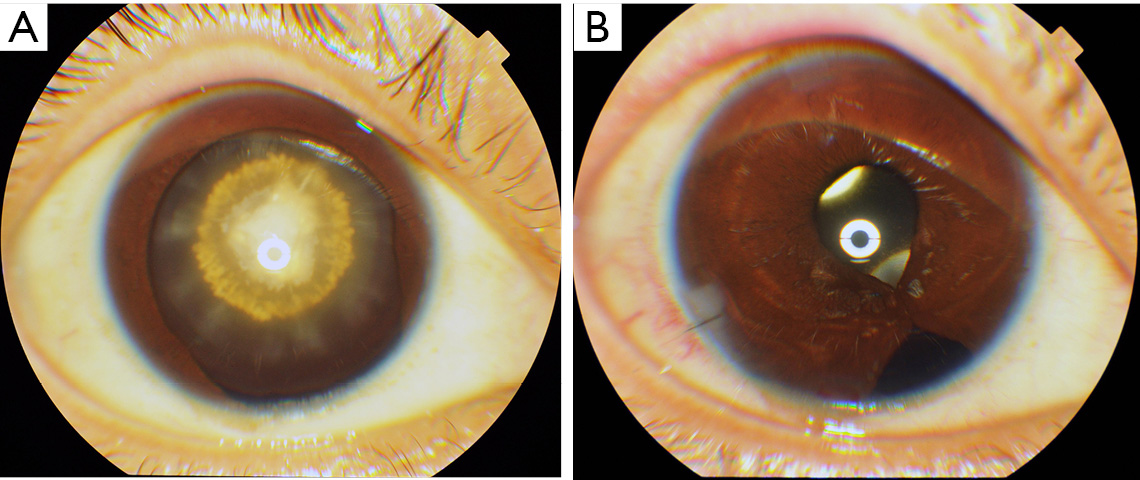
Six patients underwent simplified pupilloplasty technique between June 2013 and June 2016. Patient ages ranged between 12 to 41 years (median, 21.5 years). There were 3 male patients and 2 right eyes. Follow-up ranged from 6 to 32 months (median, 22 months). Four patients diagnosis iris coloboma and two patients induced by trauma. All the six patients combined with cataract and one patient had choroid coloboma at the same time. The iris defect ranged from 60° to 120°. Four patients presented “Keyhole” pupil and two patients presented oval pupil preoperative. Five patients complained mild to moderate photophobia and three patients had a symptom of mild glare preoperative. One patient complained monocular diplopia. All the operated eyes quickly recovered with central round pupil (Figure 2), increased visual acuity, disappeared symptoms of photophobia and glare, mild inflammation, and without major complications (Table 1).
| Variables | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
|---|---|---|---|---|---|---|
| Sex | Male | Female | Male | Female | Female | Male |
| Age (years) | 33 | 12 | 15 | 21 | 41 | 22 |
| Follow-up (months) | 6 | 28 | 23 | 32 | 15 | 21 |
| Eye | OD | OS | OS | OD | OS | OS |
| Vision (BCVA) | ||||||
| Preop | FC/40 cm | 0.02 | HM/50 cm | 0.06 | FC/40 cm | FC/60 cm |
| Postop | 0.4 | 0.8 | 0.6 | 0.8 | 0.25 | 0.6 |
| Etiology | Coloboma | Coloboma | Traumatic | Coloboma | Traumatic | Coloboma |
| Ocular and systemic associations | Cataract, choroid coloboma | Cataract | Cataract | Cataract | Cataract | Cataract |
| Range of iris defect (°) | 120 | 90 | 60 | 60 | 80 | 90 |
| Pupil shape | ||||||
| Preop | Keyhole | Keyhole | Oval | Oval | Keyhole | Keyhole |
| Postop | Round | Round | Round | Round | Round | Round |
| Pupil position | ||||||
| Preop | Inferior | Inferonasal | Inferotemporal | Inferonasal | Inferotemporal | Inferior |
| Postop | Center | Center | Center | Center | Center | Center |
| Photophobia | ||||||
| Preop | Moderate | Mild | No | Mild | Mild | Mild |
| Postop | No | No | No | No | No | No |
| Glare | ||||||
| Preop | Mild | Mild | No | No | No | Mild |
| Postop | No | No | No | No | No | No |
| Monocular diplopia | ||||||
| Preop | No | No | No | No | No | Mild |
| Postop | No | No | No | No | No | No |
| Amblyopia | Mild | No | No | No | Mild | Mild |
| Complications | No | No | No | No | No | No |
Congenital iris coloboma or traumatic iris defect is not uncommon in clinical practice. Iris defects can cause not only light sensitivity and glare but may also cause monocular diplopia and shadow images. Iris defect can be classified according to four factors: (I) the symptomatic complaints that the defect causes for the patient; (II) the relative health of remaining iris anatomy (if any); (III) the options and resources available to the patient (and his or her surgeon); and, lastly, (IV) the patient’s desired choice among available options. Surgical intervention are usually required when the patient have symptomatic complaints . An iris prosthesis are usually demanded when the iris deficiency is huge. However, suture repair may be desired when a defect is small and residual iris tissue is normal (6). The techniques used for performing pupilloplasty have evolved over the past 30 years. Although the McCannel (7) and Siepser (9) knots have been invaluable in allowing these procedures to be performed in the closed chamber. However, at least two or three corneal stab incisions are required in those technique and therefore there are more opportunities of corneal damage, iris prolapse and adhesion. In addition, another little flaw is that the line knot is easy to loose when hooking line and the suture tension cannot adjust freely. An injectable shape memory technique and instrumentation was introduced by Erlanger (11) in 2012 and it seems far easier and less time consuming than any of the conventional techniques. However, this technique is still not applied to clinical practice.
The simplified pupilloplasty technique we describe addresses the etiology of iris defect and pupil eccentricity. As far as our knowledge, this technique has two small advantages. First, all operations require only one corneal paracentesis and it decrease the opportunity of corneal damage, iris prolapse and adhesion. Second, the first time two knots bought make it not easy to slide when hooking distal line and the suture tension can be adjusted freely according to needs. On the other hand, negligible complications and mild inflammation presented after a mean follow-up time of 10 months (range, 6–34 months). As we all know that this technique has the risk of causing iatrogenic cataracts in the presence of a transparent lens eye. However, this complication can still be avoided if enough viscoelastic agent was injected between the iris and lens, and careful operation when the needle puncture through the iris in the meanwhile.
Furthermore, we have extended the application of this technology to intraocular lens (IOL) dislocation or decentration. There no doubt that scleral suture fixation of dislocated IOL would be preferred to the exchange considering the potential complications (12). The least traumatic method to reposition the IOL is essential. Pulling out the luxated IOL may provide a fixed knot. However, it requires rotating the IOL which may lead to damage and complications. Our technique is minimally invasive in a closed system with controlled intraocular pressure (IOP) and minimizes awkward manipulations. The needle is not passed in and out of the eye several times. The first time two knots bought make it not easy to cause IOL slippage. Although we have only successfully applied this technique in only one patient who presented intraocular lens dislocation induced by trauma after penetrating keratoplasty. We are full of confidence for this expansion application of this technology in the future.
Although we have performed this technique in only a few patients, the results have been effective and reproducible. However, even with this limited experience, we can conclude that the simplified pupilloplasty technique presented here could be a good alternative for the management of small iris coloboma or traumatic iris defect. In addition, the expansion application of this technology in IOL dislocation or decentration may be attractive.