Abstract: Four challenging and unusual retinal cases: (I) 11-year follow-up for retinal hemangioblastoma with von Hippel-Lindau (VHL) disease; (II) treatment for central serous chorioretinopathy (CSC)—observation, half does photodynamic therapy (PDT) or micropulse laser photocoagulation; (III) diagnosis and treatment for a child with optic nerve defect; (IV) the optional treatment for retinal detachment (RD) with iridolenticular choroidal coloboma, were presented and discussed by three international retinal specialists at a retinal clinical round in Fundus Diseases Center of Zhongshan Ophthalmic Center (ZOC). The discussion helps us a better understanding of the pathogenesis and managements of these four retinal diseases and their association with systemic conditions.
On June 16, 2016, one day before the Zhongshan Ophthalmic Center (ZOC) Medical Retina and Epidemiology Symposium, Emily Y. Chew, Robert P. Murphy and Timothy W. Olsen, three international renowned retinal specialists and Chi-Chao Chan, international famous ophthalmic pathologist, were invited to attend a retinal clinical round in Fundus Diseases Center of ZOC. Four challenging and unusual retinal cases were presented and discussed during the clinical round. Clinical pearls derived from these four cases were summarized.
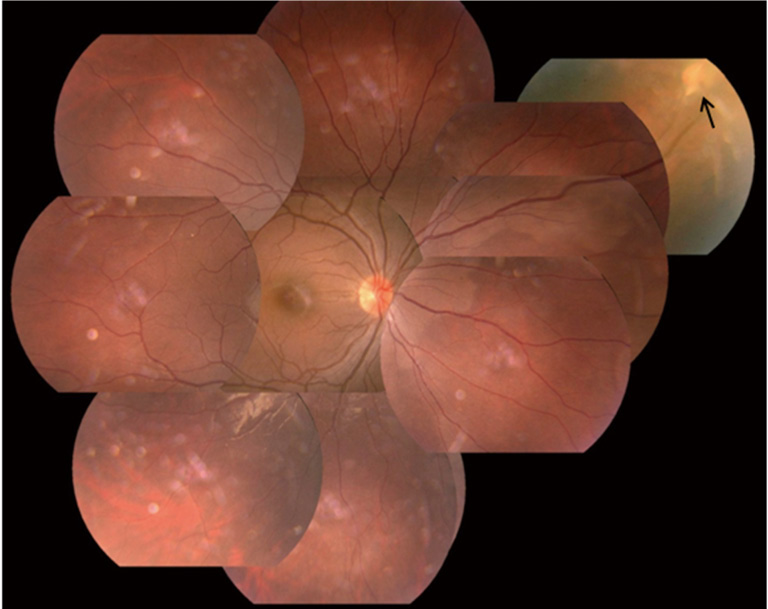
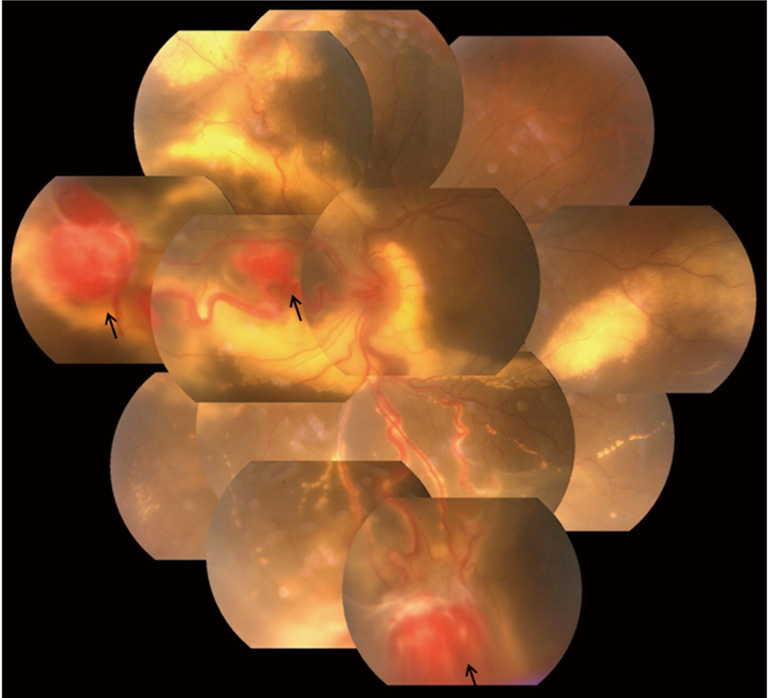
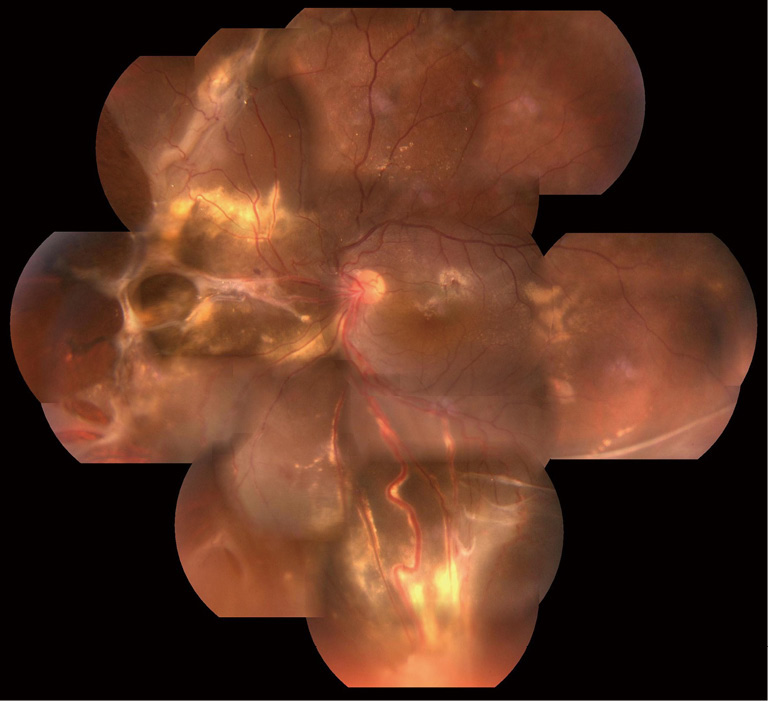
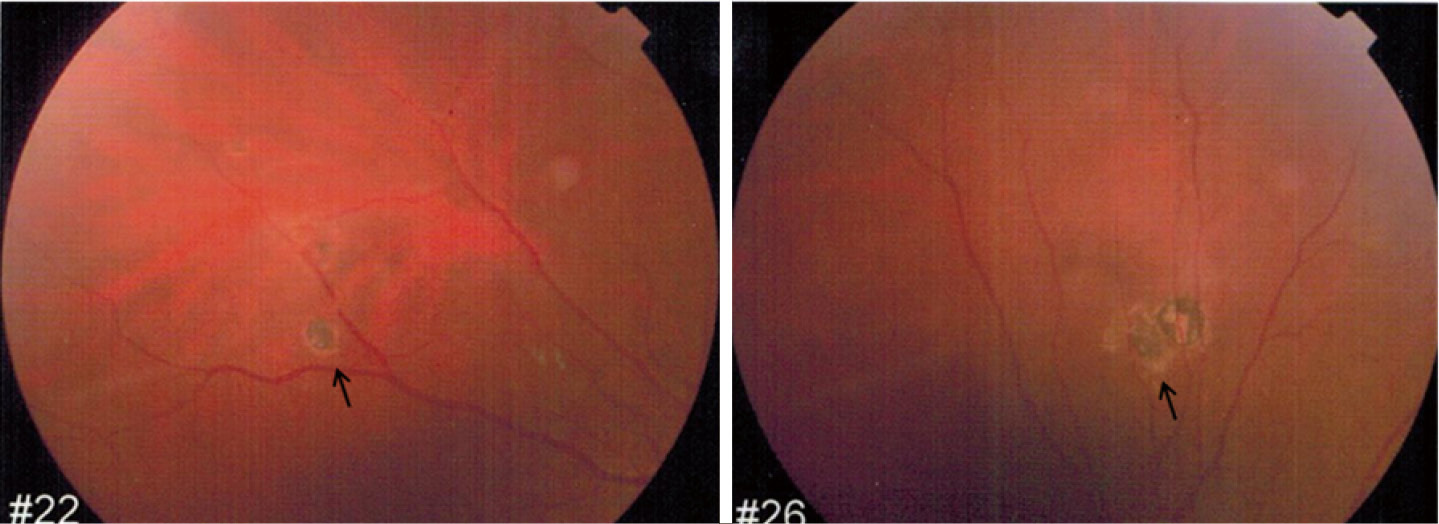
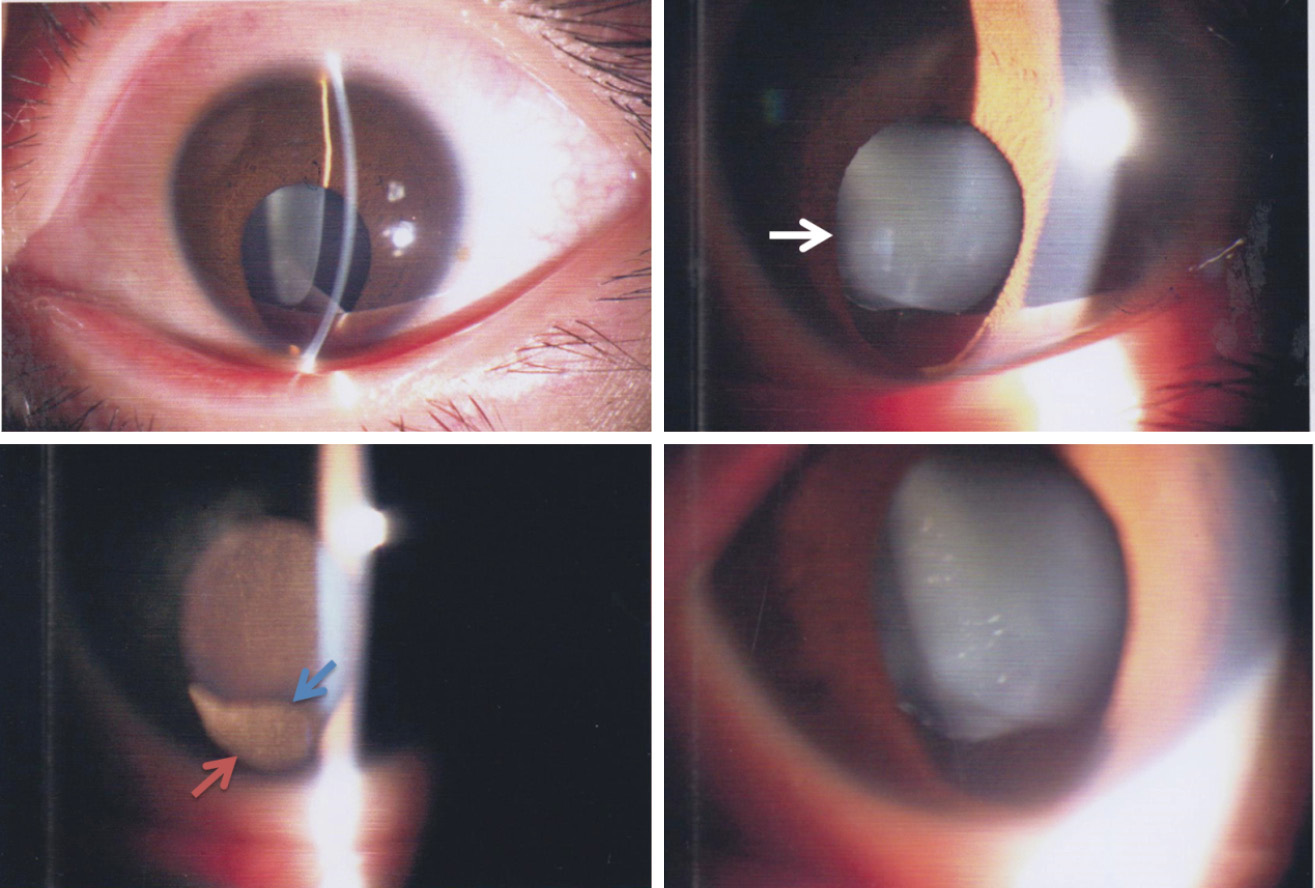
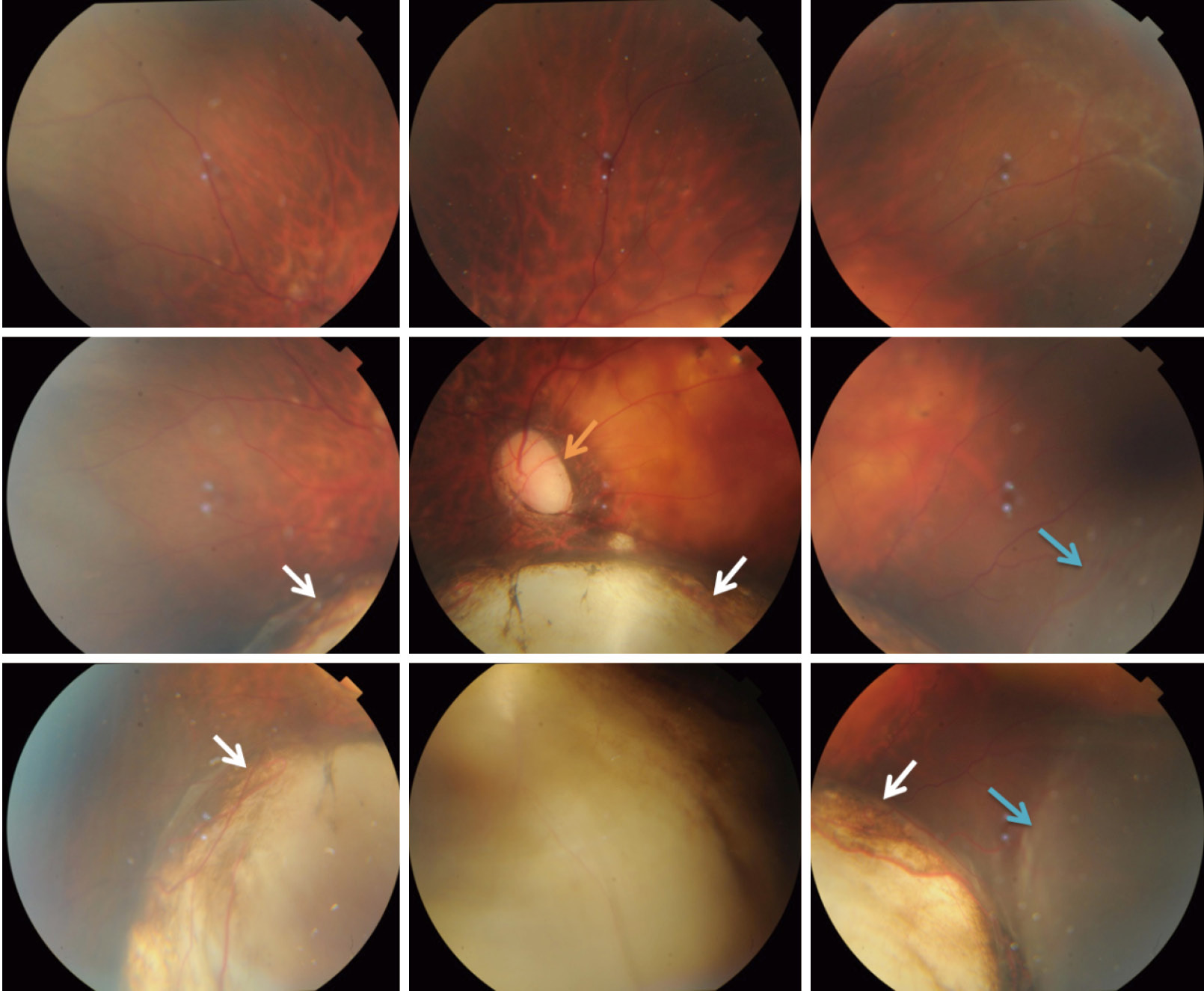
Eleven years ago, in 2005, a 20-year-old female with familial von Hippel-Lindau (VHL) disease complained of progressive loss of visual acuity and defection of superior visual field in her left eye for 6 months. She had no systemic manifestations at her first visit to ZOC. Her father had retinal hemangioblastoma in both eyes; her paternal uncle and aunt had histories of cerebellar hemangioblastoma. Her vision was 1.2 (20/16) in the right eye and 0.4 (20/50) in the left eye. Anterior segment was normal in both eyes. There was a small retinal hemangioblastomas in the superior nasal periphery of the right eye (Figure 1). Three large retinal hemangioblastomas with dilated feeder vessels surrounded by serous detachment, as well as multiple hard and soft exudates, were seen in the nasal and inferior peripheries of the left eye (Figure 2). A few tiny retinal hemangioblastomas also were noted in the periphery. Tractional and exudative retinal detachment (RD) in the inferior periphery as well as macular edema was observed at the time of presentation. The small retinal hemangioblastomas in both eyes were treated with laser photocoagulation. Later, the patient successfully underwent pars plana vitrectomy (PPV), resection of the largest nasal hemangioblastoma, endolaser photocoagulation, endodiathermy, and silicone oil tamponade in the left eye. Three months after surgery, flat retina and the resection sites of the nasal retinal hemangioblastomas were observed in the left eye (Figure 3). Unfortunately, due to the formation of epiretinal membrane and recurrent RD in the inferior retina, her macula remained edematous and her vision worsened gradually 6 months after surgery. Cataract surgery was performed on the left eye 2 years after PPV while the silicone oil remained inside. And 11 years later, at the latest follow-up, her vision of the right eye remained at 1.2 (20/16) and the left was light perception. Anterior segment is normal, and no new retinal hemangioblastoma was found in the right eye, dystrophy of the retinal hemangioblastoma after laser photocoagulation was showed (Figure 4). But in the left eye, posterior capsular opacity, epiretinal membrane and RD in the inferior periphery was found. During the long-time follow-up, some systemic disorders developed. In 2012 renal cysts was found in her left kidney and micro invasive operation was performed. In 2013 cerebellar hemangioblastoma was confirmed, but it was small and stable and still under observation.
All retinal specialists agreed that case 1 was a typical case of retinal hemangioblastomas associated with VHL disease. Professor Chew, an expert in this rare disease, stated that retinal and central nerve system (CNS) hemangioblastomas are the most common manifestations, and are frequently the earliest signs of VHL disease (1). She suggested that laser photocoagulation could fully treat small retinal hemangioblastomas as showed in this case (2). Professor Xiaoling Liang, the attending ophthalmologist of this case, and Professor Chenjin Jin, specialist in laser photocoagulation, presented their techniques and experiences of photocoagulation for retinal hemangioblastoma associated with VHL disease. Professor Chan mentioned that large hemangioblastomas could be treated successfully with plaque radiotherapy or surgical resection of the retinal angiomas (3,4), but plaque radiotherapy is not available in China currently; thus, surgical resection is the treatment of choice for large retinal hemangioblastomas that do not respond to photocoagulation and cryotherapy. Professor Olsen believed that resection of the large retinal hemangioblastoma by PPV in this case was a challenging procedure. Although cataract and recurrent RD occurred in the long term, the operation extended visual quality time of the left eye to this patient. Professor Murphy emphasized the importance of medical surveillance for this patient because VHL disease is a multisystem neoplastic syndrome (5).
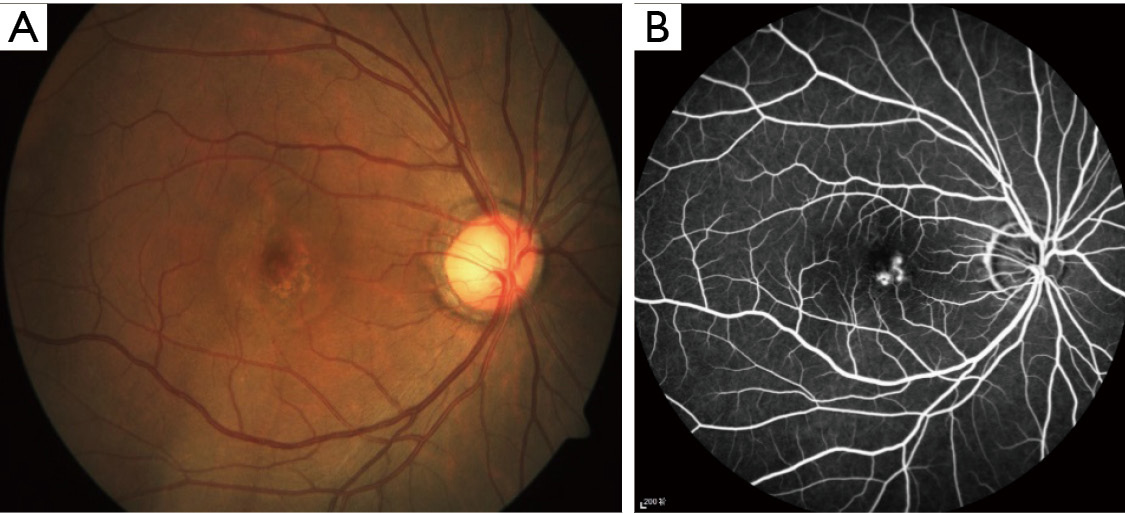
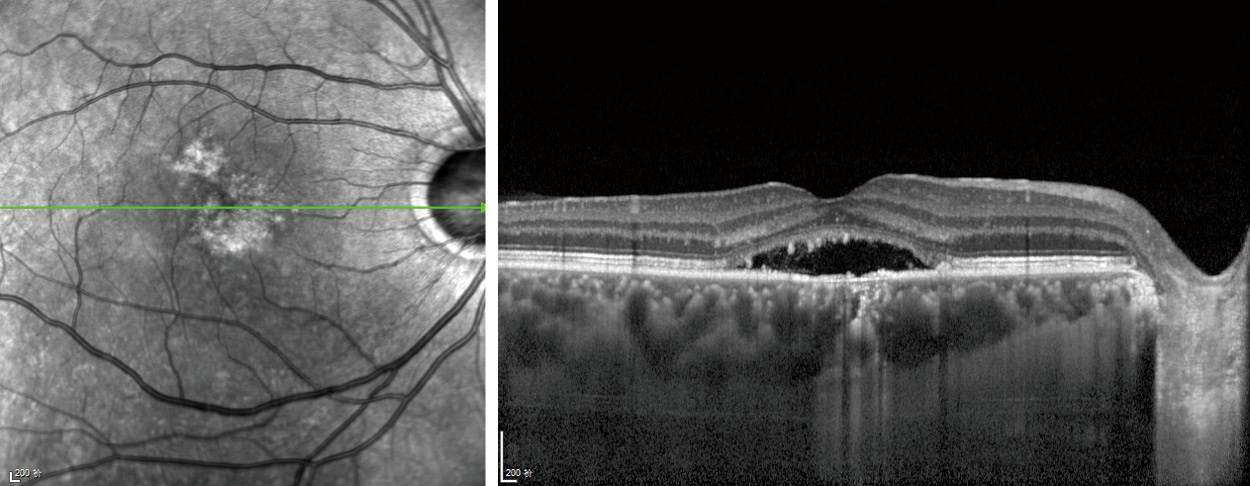
A 41-year-old man presented to ZOC with complaining of decreased visual acuity of the right eye for 6 months. There was no improvement of visual acuity after taking traditional Chinese medicine in a local hospital. There was no other eye disease history or systematic disease. Best corrected visual acuity (BCVA) was 0.5 (20/40) in right eye and 1.0 (20/20) in left eye. Intraocular pressure was normal in both eyes. No abnormality was found in the anterior segment. Serous detachment of sensory retina and pigmented changes were found in macular area and fundus fluorescence angiography (FFA) showed focal leakage near fovea of the right eye (Figure 5). Subretinal fluid (SRF) with small gray-white subretinal precipitates and rough retinal pigment epithelium (RPE) layer in macula were seen on optical coherence tomography (OCT) (Figure 6). Based on the above examinations, chronic central serous chorioretinopathy (CSC) in the right eye was diagnosed. Half-dose photodynamic therapy (PDT) was performed for his right eye after informed consent was obtained. However, persistent SRF was found at the 1-, 3- and 6-month follow-up (Figure 7). BCVA remained 0.5 (20/40). Meanwhile, macular sensitivity was decreased gradually. At this time, we advised the patient to take the second-time half-dose PDT. But he rejected our advice for economic reason and received the subthreshold micropulse laser photocoagulation (SMLP). The parameter of SMLP was as follows: model, micropulse model; duty cycle, 5%; exposure time, 200 ms; laser spots, 100 μm; power, 675 mw (50% of titration power). Three months after the SMLP treatment, SRF was absorbed completely on OCT images (Figure 8), and macular sensitivity improved from 14.6 to 25.6 dB (Figure 9) and BCVA increased to 1.0 (20/20). No obvious retinal damage could be observed on fundus autofluorescence (FAF) images.
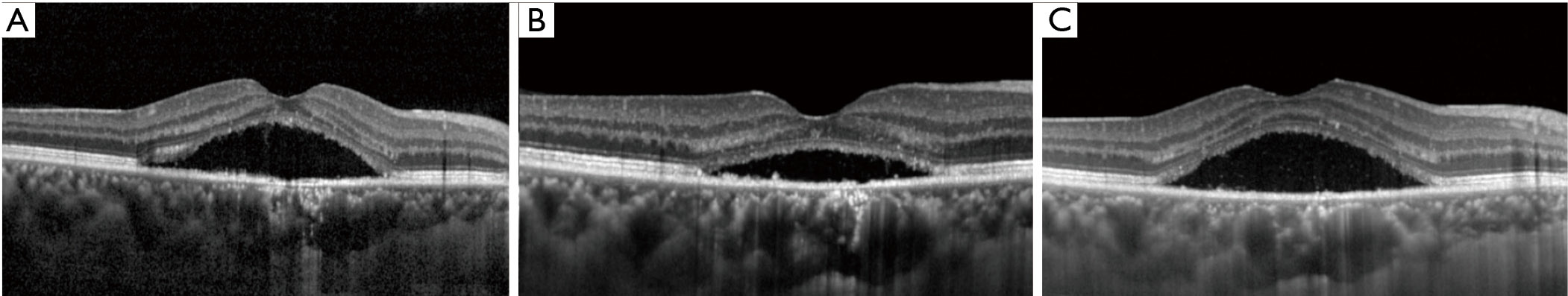
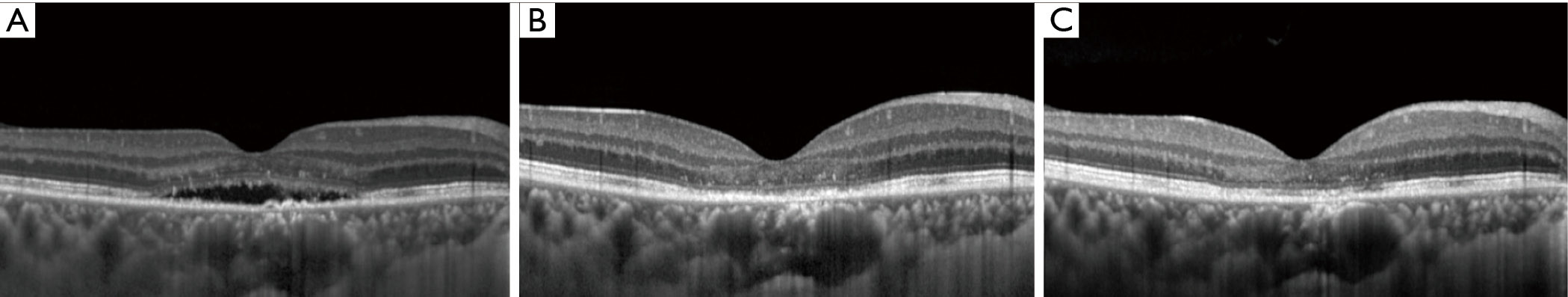
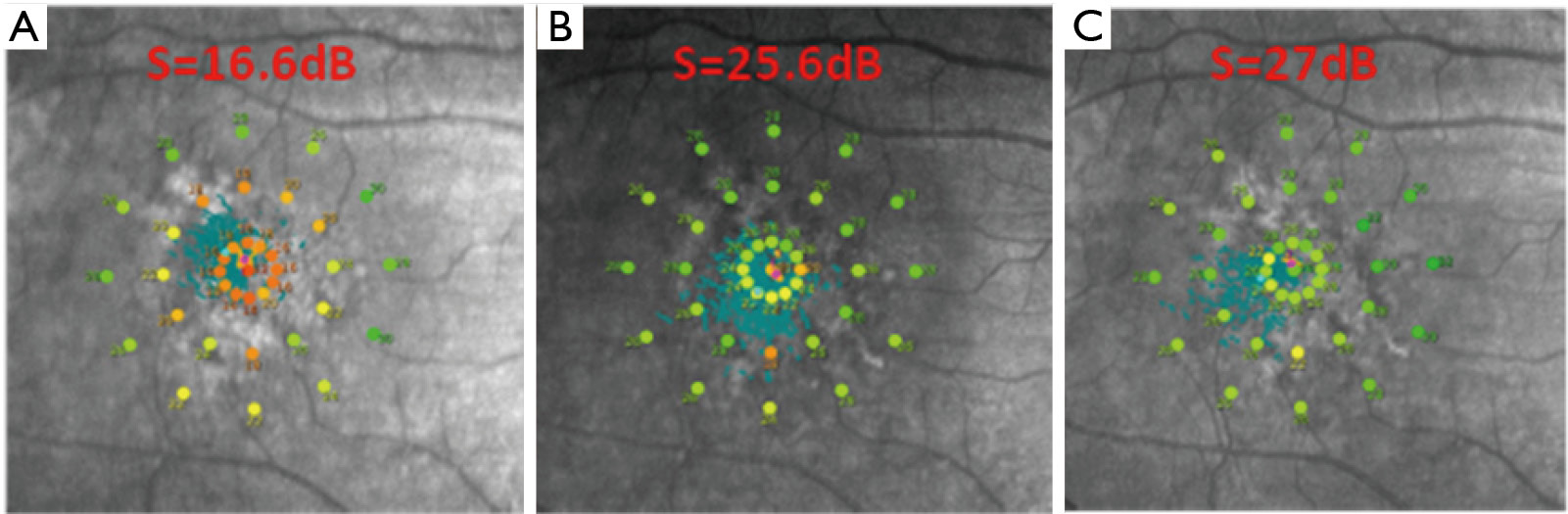
Chronic CSC is a common macular disease in younger adult and often leads to visual impairment due to retinal neurosensory detachment and RPE damage (6). Conventional laser photocoagulation can shorten duration and accelerate the resolution of the SRF, while this treatment is not suitable for macular leaking spot near fovea (7). So far, half-dose PDT is the first line treatment in the leakage spots close to fovea for chronic CSC (8,9). However, there is no answer to how to treat the chronic CSC with persistent SRF after PDT, just like this case. Professors Murphy and Olsen agreed that the advent of SMLP enriched the options for the treatment of CSC (10,11). Professor Jin, the attending ophthalmologist of this case, believed that the experience in this case showed SMLP was a potential option for CSC without obvious retinal damage. SMLP is a novel laser delivery modality for the retinal disease treatment in recent years. Professor Jin described that in the micropulse model, laser energy is dispensed in a burn or envelope of micropulse that consists of the “ON” time and the “OFF” time. The “ON” time is the duration of each micropulse and the “OFF” time between successive micropulse allows the heat to cool down, which can minimize the heat destruction to the adjacent tissue (12). In this case, through the SMLP treatment, the patient with persistent SRF after PDT got satisfactory anatomy and visual function improvement. In a word, SMLP has many advantages, for example, inexpensive, repeating treatment and no obvious damage to retina. It may be a good option for the treatment of persistent SRF of CSC after PDT (13), especially for those with leaking spot near fovea.
A 6-year-old boy with a chief complaint of poor vision in his left eye for over one month was presented to ZOC. The boy is a full-term baby given birth by caesarean section. He had a medical history of thalassemia. His family members were claimed healthy. The corrected visual acuity was 0.5 (20/40) on the right and no light perception on the left. Intraocular pressure was 11 mmHg on the right and 14 mmHg on the left. In the left eye, mydriasis and disappeared direct light reflex was observed without nystagmus and strabismus (Figure 10). Bilateral optic disks were enlarged and pale (Figure 11). Ultrasound biomicroscopy (UBM) showed open angle of the anterior chamber in both eyes; ultrasonography showed normal axial length of both eyes; FFA showed no obvious leakage in early and late phase; OCT showed a cyst cavity in the left macular neurosensory layer; ANGIO OCT showed disconnected blood vessels in bilateral optic disk and narrower blood vessels in the left eye; visual evoked potentia (VEP) showed PVEP reaction of each box was severely abnormal on the right and FVEP reaction was severely abnormal on the left; electroretinogram (ERG) showed normal reaction of rod cells ; slightly abnormal reaction of cone cells on the right and slightly abnormal reaction of rod cells ; moderately abnormal reaction of cone cells on the left. Furthermore, craniocerebral imageology examinations were applied: magnetic resonance imaging (MRI) showed partly empty sella turcica, Galen venous malformation and choroidal fissure cyst; neuro high resolution MRI showed thin optic nerve and maldevelopment of olfactory bulb, olfactory cleft and olfactory tract. Blood and urine tests showed microcytic hypochromic anemia, low FSH, LH, and testosterone level and positive urine protein. The boy’s appearance was special: deep eye socket and a squared skull (Figure 12); curving left index finger and wide gap between toes.
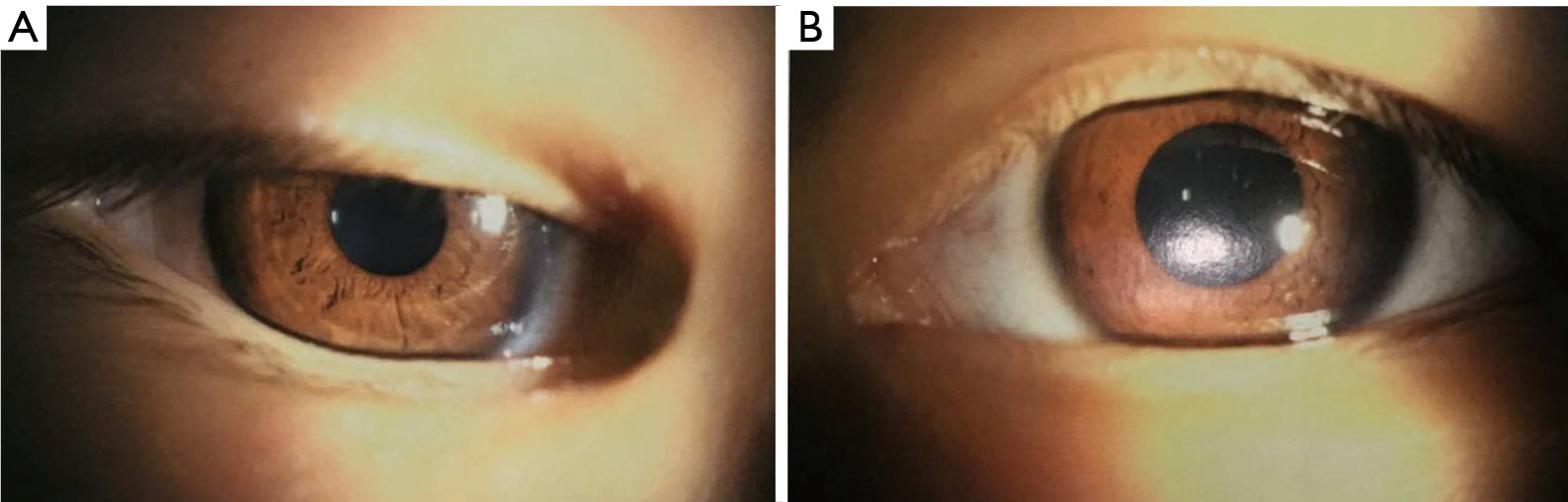
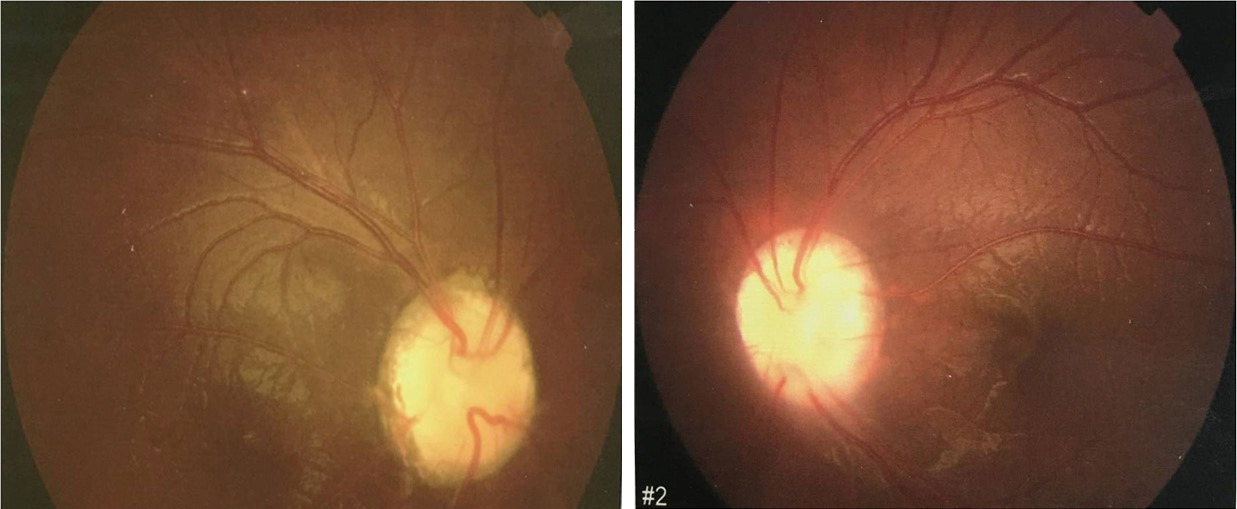
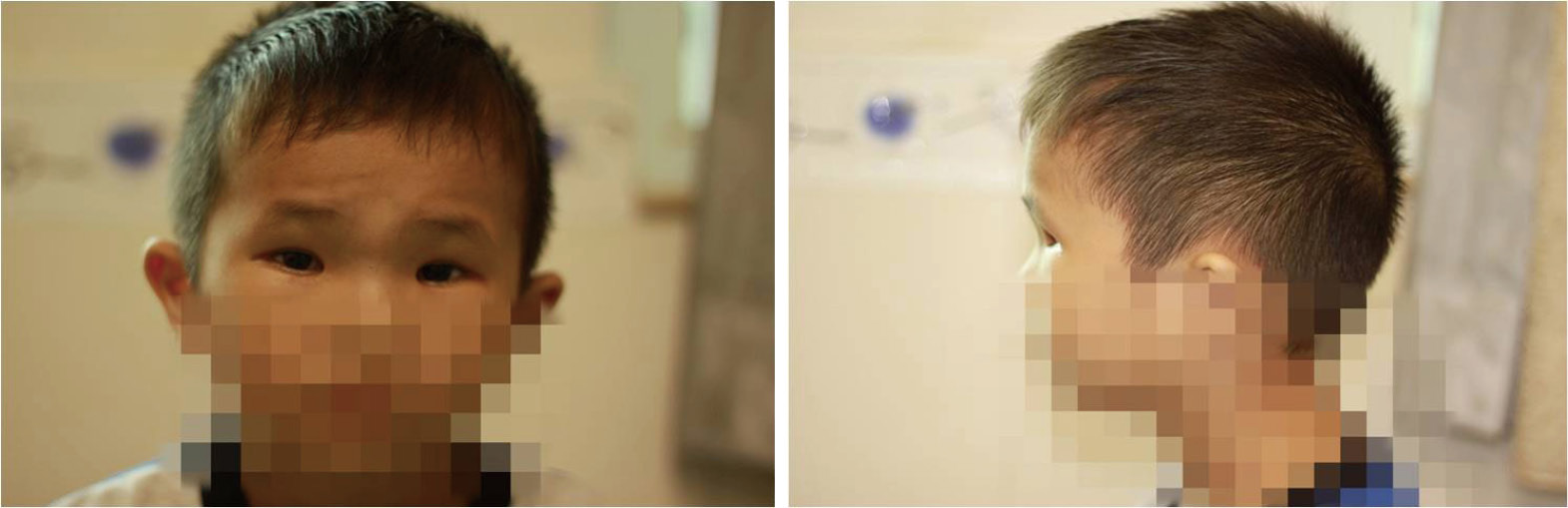
All the retinal specialists in the clinical round agreed that it was a very challenging case with a presumptive diagnosis of “optic disk coloboma combining with optic nerve hypoplasia” and some systemic abnormalities. Professor Jie Hu, the attending ophthalmologist of this case, explained that the positive findings of this boy aroused our thought that whether the abnormity is with a kind of possible syndrome (such as Kallmann syndrome or septo-optic dysplasia, etc.) or a primary optic disc coloboma combining with optic nerve dysplasia. All the syndromes mentioned above have some matched points and some discrepant points: Kallmann syndrome also have maldevelopmented of olfactory bulb, olfactory cleft and olfactory tract and low gonadal hormone level (14). However, no ocular complications were ever reported in Kallmann syndrome and this boy’s sense of smell was normal; septo-optic dysplasia can also have optic nerve hypoplasia, endocrine disorders and partly empty sella turcica (15). Interestingly, no sign of septum pellucidum agenesis were found in MRI and only gonadal hormone were affected. Professors Chew, Murphy and Olsen all emphasized that when we meet patients having optic nerve hypoplasia, we should be sensitive to the underlying abnormalities of the central nervous system and abnormal hormone level. Professor Chi-Chao Chan suggested to consult with Dr. Brian Brooks of National Eye Institute, National Institutes of Health, an expert in ocular coloboma (16). Dr. Brooks advised to follow-up the patient’s renal function because these patients would have a greater chance developing nephropathy.
A 26-year-old woman presented to ZOC with decreased vision of her left eye for several years and got worse for 2 weeks. Her right eye had been blind since her childhood. No ophthalmic past history or family history had been mentioned. On examination, the BCVA was no light perception in the right eye (OD) and 0.1 (20/200) in the left eye (OS). The intraocular pressure was 10.0 mmHg OD and 12.3 mmHg OS. There was microcornea and corneal leucoma in the right eye. The ocular abnormalities of the left eye included inferior iris coloboma, cataracts with specific inferior lens notching and lens zonule disruption (Figure 13), optic disc atrophy and inferior choroidal coloboma (Figure 14). The B-scan ultrasonography of the left eye showed a RD. The 23 G pars planar lensectomy and vitrectomy, drainage retinotomy, heavy liquid, endolaser, peripheral iridotomy, heavy liquid-air exchange and air-silicone oil exchange was performed. No retinal break was found during the surgery. Her retina remained attached up to the last visit (two weeks postoperatively).
Congenital iridolenticular choroidal coloboma is a rare condition caused by failure of the optic fissure to close (17). This case was a classic defect including partial absence of the inferior quadrant of the iris, choroid, and retina. Surgical treatment was necessary for dealing with the complications of cataract and RD (18). The surgical options of this case were discussed. Pars planar vitrectomy was recommended as the primary choice (19). Prof. Olsen suggested meticulous releasing vitreous traction at the disc and coloboma, carefully searching of the retinal break, and barricading endolaser onto the edge of coloboma. The peripheral iridotomy was not recommended, because of the existing inferior iris coloboma. Professor Lin Lu, the chief director of Fundus Diseases Center of ZOC, specialist in vitreous surgery, thought that primary cataract surgery was only needed if the lens opacity interfered the view of vitrectomy. Silicone oil tamponade was approved in this case. But the caution of silicone oil shifting through the optic nerve tube was mentioned, since there was optic disc atrophy in this case. The duration of silicone oil tamponade was recommended for 3–6 months or longer, considering of the difficulty of retina adherence of the edge of the coloboma.
Over all, the discussion of these four challenging and unusual retinal cases allow us better understanding of the complexity of the fundus diseases, the relationship between fundus and systemic disorders, and the difficulties of managing these cases.