1、Margo CE, Hamed LM. Ocular syphilis. Surv Ophthalmol 1992;37:203-20.
2、Benson CE, Soliman MK, Knezevic A, et al. Bilateral papillitis and unilateral focal chorioretinitis as the presenting features of syphilis. J Ophthalmic Inffamm Infect 2015;5:16.
3、Lee SB, Kim KS, Lee WK, et al. Ocular syphilis characterised by severe scleritis in a patient infected with HIV. Lancet Infect Dis 2013;13:994.
4、Bonnin N, Laurichesse H, Beytout J, et al. Ophthalmologists play a key role in the management of syphilis presenting with ocular involvement. Acta Ophthalmol 2014;92:e328-9.
5、Pan SW, Yusof NS, Hitam WH, et al. Syphilitic uveitis: report of 3 cases. Int J Ophthalmol 2010;3:361-4.
6、Yang B, Xiao J, Li X,et al. Clinical manifestations of syphilitic chorioretinitis: a retrospective study. Int J Clin Exp Med 2015;8:4647-55.
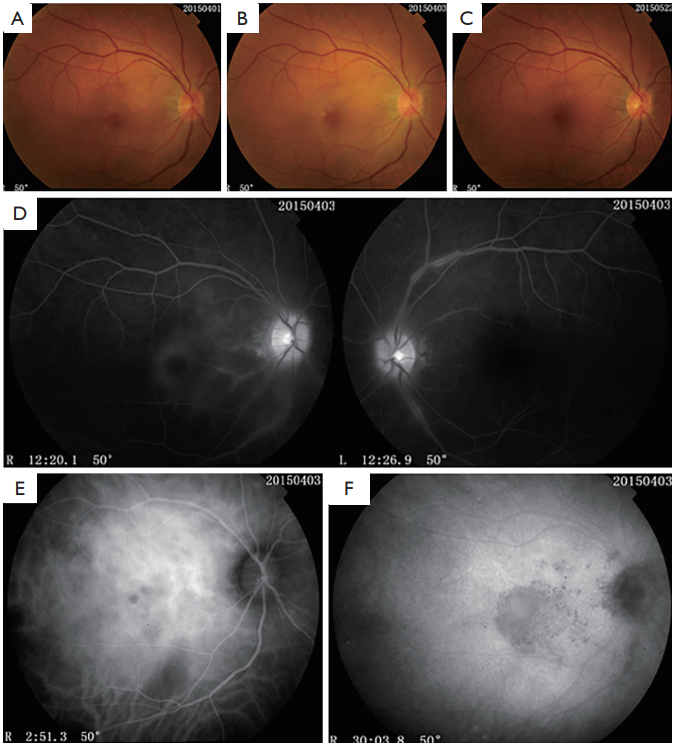
7、Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology 1990;97:1288-97.
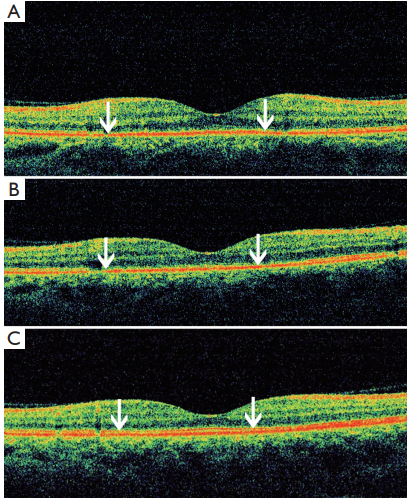
8、Burkholder BM, Leung TG, Ostheimer TA, et al. Spectral domain optical coherence tomography ffndings in acute syphilitic posterior placoid chorioretinitis. J Ophthalmic
Inflamm Infect 2014;4:2.
9、de Souza EC, Jalkh AE, Trempe CL, et al. Unusual central chorioretinitis as the ffrst manifestation of early secondary syphilis. Am J Ophthalmol 1988;105:271-6.
10、Samson CM, Foster CS. Syphilis. In: Foster CS, Vitale AT, editors. Diagnosis and Treatment of Uveitis. Philadelphia: WB Saunders. 2001:237-43. chap.15.
11、Baglivo E, Kapetanios A, Safran AB. Fluorescein and indocyanine green angiographic features in acute syphilitic macular placoid chorioretinitis. Can J Ophthalmol 2003;38:401-5.
12、Teplinskaia%20LE%2C%20Kaliberdina%20AF%2C%20Za%C4%ADtseva%20NS%2C%20et%20al.%20Clinical-immunological%20disorders%20in%20uveitis%20in%20patients%20with%20Beh%C3%A7et's%20syndrome.%20Vestn%20Oftalmol%201994%3B110%3A23-5.
13、Lee MI, Lee AW, Sumsion SM, et al. Don't Forget What You Can't See: A Case of Ocular Syphilis. West J Emerg Med 2016;17:473-6.
14、Benhamou N, Souied EH, Zolf R, et al. Adult-onset foveomacular vitelliform dystrophy: a study by optical coherence tomography. Am J Ophthalmol 2003;135:362-7.