1、Hou X, Wang L, Zhu D, et al. Prevalence of diabetic retinopathy and
vision-threatening diabetic retinopathy in adults with diabetes in
China[ J]. NatCommun, 2023, 14(1): 4296. DOI: 10.1038/s41467-
023-39864-w.Hou X, Wang L, Zhu D, et al. Prevalence of diabetic retinopathy and
vision-threatening diabetic retinopathy in adults with diabetes in
China[ J]. NatCommun, 2023, 14(1): 4296. DOI: 10.1038/s41467-
023-39864-w.
2、Chua J, Lim CXY, Wong TY, et al. Diabetic retinopathy in the asia�pacific[ J]. Asia PacJ Ophthalmol, 2018, 7(1): 3-16. DOI: 10.22608/
APO.2017511.Chua J, Lim CXY, Wong TY, et al. Diabetic retinopathy in the asia�pacific[ J]. Asia PacJ Ophthalmol, 2018, 7(1): 3-16. DOI: 10.22608/
APO.2017511.
3、Shao Y, Zhou Q. Interpretation of clinical guidelines for diabetic
retinopathy of the American Academy of Ophthalmology 2018[ J].
Recent Advances in Ophthalmology, 2019, 39(06): 501-506. DOI:
10.13389/j.cnki.rao.2019.0115.Shao Y, Zhou Q. Interpretation of clinical guidelines for diabetic
retinopathy of the American Academy of Ophthalmology 2018[ J].
Recent Advances in Ophthalmology, 2019, 39(06): 501-506. DOI:
10.13389/j.cnki.rao.2019.0115.
4、Gologorsky D, Thanos A, Vavvas D. Therapeutic interventions against
inflammatory and angiogenic mediators in proliferative diabetic
retinopathy[ J]. Mediators Inflamm, 2012, 2012: 629452. DOI:
10.1155/2012/629452.Gologorsky D, Thanos A, Vavvas D. Therapeutic interventions against
inflammatory and angiogenic mediators in proliferative diabetic
retinopathy[ J]. Mediators Inflamm, 2012, 2012: 629452. DOI:
10.1155/2012/629452.
5、Huang H, Gandhi JK, Zhong X, et al. TNF alpha is required for late
BRB breakdown in diabetic retinopathy, and its inhibition prevents
leukostasis and protects vessels and neurons from apoptosis[ J]. Invest
Ophthalmol VisSci, 2011, 52(3): 1336-1344. DOI: 10.1167/iovs.10-
5768.Huang H, Gandhi JK, Zhong X, et al. TNF alpha is required for late
BRB breakdown in diabetic retinopathy, and its inhibition prevents
leukostasis and protects vessels and neurons from apoptosis[ J]. Invest
Ophthalmol VisSci, 2011, 52(3): 1336-1344. DOI: 10.1167/iovs.10-
5768.
6、Adamis AP, Berman AJ. Immunological mechanisms in the pathogenesis
of diabetic retinopathy[ J]. SeminImmunopathol, 2008, 30(2): 65-84.
DOI: 10.1007/s00281-008-0111-x.Adamis AP, Berman AJ. Immunological mechanisms in the pathogenesis
of diabetic retinopathy[ J]. SeminImmunopathol, 2008, 30(2): 65-84.
DOI: 10.1007/s00281-008-0111-x.
7、Tang L, Xu GT, Zhang JF. Inflammation in diabetic retinopathy: possible
roles in pathogenesis and potential implications for therapy[ J]. Neural
Regen Res, 2023, 18(5): 976-982. DOI: 10.4103/1673-5374.355743.Tang L, Xu GT, Zhang JF. Inflammation in diabetic retinopathy: possible
roles in pathogenesis and potential implications for therapy[ J]. Neural
Regen Res, 2023, 18(5): 976-982. DOI: 10.4103/1673-5374.355743.
8、苏陆青, 周炳娟, 张月玲, 等. 糖尿病视网膜病变发病机制的研
究进展[ J]. 医学研究与教育, 2011, 28(4): 74-77. DOI: 10.3969/
j.issn.1674-490X.2011.04.020.
Su LQ, Zhou BJ, Zhang YL, et al.Research progress on the pathogenesis
of diabetic retinopathy[ J]. Med Res Educ, 2011, 28(4): 74-77. DOI:
10.3969/j.issn.1674-490X.2011.04.020.Su LQ, Zhou BJ, Zhang YL, et al.Research progress on the pathogenesis
of diabetic retinopathy[ J]. Med Res Educ, 2011, 28(4): 74-77. DOI:
10.3969/j.issn.1674-490X.2011.04.020.
9、易茜璐, 于明香. 糖尿病视网膜病变的发病机制[ J]. 复旦学
报(医学版), 2010, 37(5): 604-607. DOI: 10.3969/j.issn.1672-
8467.2010.05.024.
Yi QL, Yu MX. Pathogenesis of diabetic retinopathy[ J]. Fudan
Univ J Med Sci, 2010, 37(5): 604-607. DOI: 10.3969/j.issn.1672-
8467.2010.05.024.Yi QL, Yu MX. Pathogenesis of diabetic retinopathy[ J]. Fudan
Univ J Med Sci, 2010, 37(5): 604-607. DOI: 10.3969/j.issn.1672-
8467.2010.05.024.
10、Demircan N, Safran BG, Soylu M, et al. Determination of vitreous
interleukin-1 (IL-1) and tumour necrosis factor (TNF) levels in
proliferative diabetic retinopathy[ J]. Eye, 2006, 20(12): 1366-1369.
DOI: 10.1038/sj.eye.6702138.Demircan N, Safran BG, Soylu M, et al. Determination of vitreous
interleukin-1 (IL-1) and tumour necrosis factor (TNF) levels in
proliferative diabetic retinopathy[ J]. Eye, 2006, 20(12): 1366-1369.
DOI: 10.1038/sj.eye.6702138.
11、Abcouwer SF. Angiogenic factors and c y tokines in diabetic
retinopathy[ J]. JClinCellImmunol, 2013, Suppl 1(11): 1-12. DOI:
10.4172/2155-9899.Abcouwer SF. Angiogenic factors and c y tokines in diabetic
retinopathy[ J]. JClinCellImmunol, 2013, Suppl 1(11): 1-12. DOI:
10.4172/2155-9899.
12、Marwaha AK, Crome SQ, Panagiotopoulos C, et al. Cutting edge:
increased IL-17-secreting T cells in children with new-onset type 1
diabetes[ J]. J Immunol, 2010, 185(7): 3814-3818. DOI: 10.4049/
jimmunol.1001860.Marwaha AK, Crome SQ, Panagiotopoulos C, et al. Cutting edge:
increased IL-17-secreting T cells in children with new-onset type 1
diabetes[ J]. J Immunol, 2010, 185(7): 3814-3818. DOI: 10.4049/
jimmunol.1001860.
13、Obasanmi G, Lois N, Armstrong D, et al. Peripheral blood mononuclear
cells from patients with type 1 diabetes and diabetic retinopathy
produce higher levels of IL-17A, IL-10 and IL-6 and lower levels
of IFN-γ-apilot study[ J]. Cells, 2023, 12(3): 467. DOI: 10.3390/
cells12030467.Obasanmi G, Lois N, Armstrong D, et al. Peripheral blood mononuclear
cells from patients with type 1 diabetes and diabetic retinopathy
produce higher levels of IL-17A, IL-10 and IL-6 and lower levels
of IFN-γ-apilot study[ J]. Cells, 2023, 12(3): 467. DOI: 10.3390/
cells12030467.
14、Byrne EM, Llorián-Salvador M, Tang M, et al. IL-17A damages the
blood-retinal barrier through activating the Janus kinase 1 pathway[ J].
Biomedicines, 2021, 9(7): 831. DOI: 10.3390/biomedicines9070831.Byrne EM, Llorián-Salvador M, Tang M, et al. IL-17A damages the
blood-retinal barrier through activating the Janus kinase 1 pathway[ J].
Biomedicines, 2021, 9(7): 831. DOI: 10.3390/biomedicines9070831.
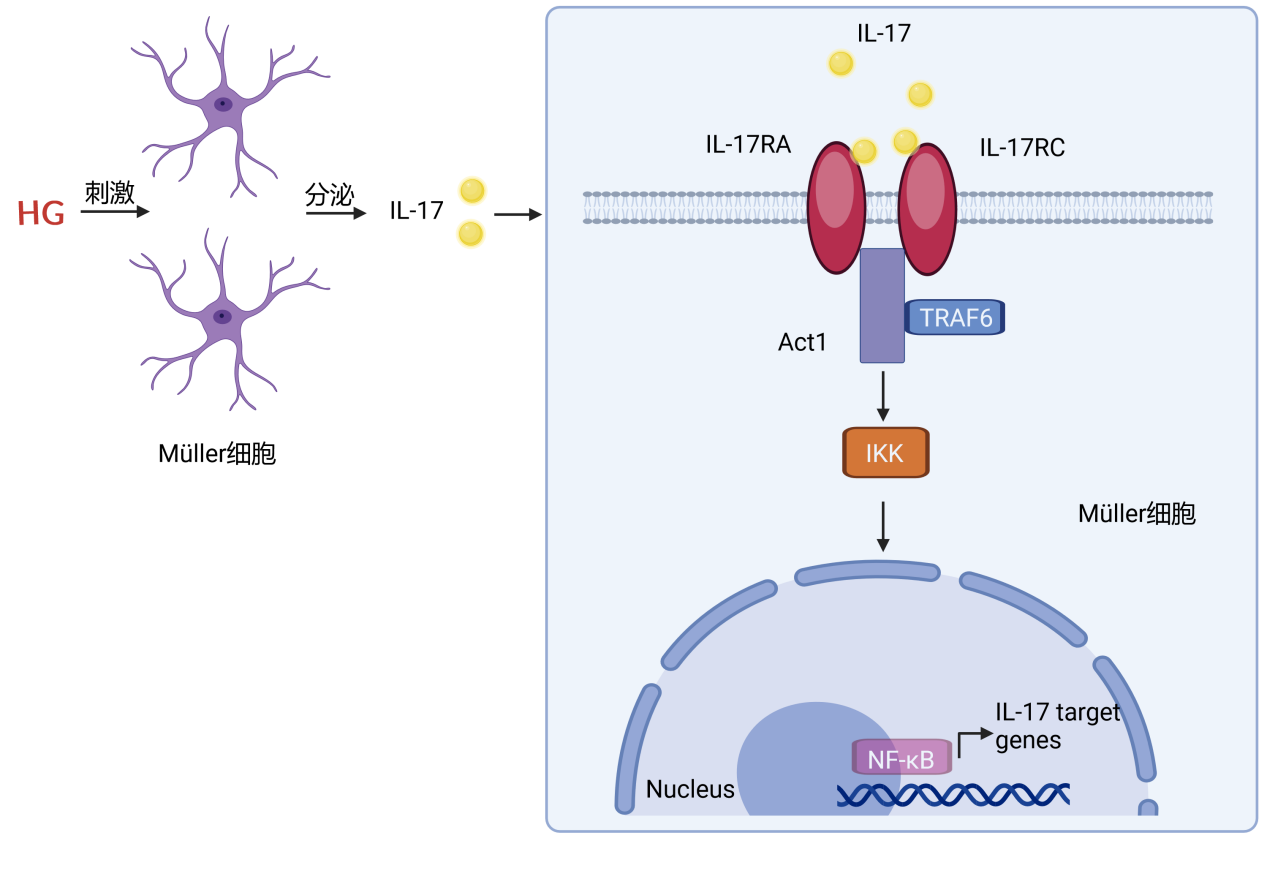
15、Qiu AW, Bian Z, Mao PA, et al. IL-17A exacerbates diabetic retinopathy
by impairing Müller cell function via Act1 signaling[ J]. Exp Mol Med,
2016, 48(12): e280. DOI: 10.1038/emm.2016.117.Qiu AW, Bian Z, Mao PA, et al. IL-17A exacerbates diabetic retinopathy
by impairing Müller cell function via Act1 signaling[ J]. Exp Mol Med,
2016, 48(12): e280. DOI: 10.1038/emm.2016.117.
16、Bringmann A, Pannicke T, Grosche J, et al. Müller cells in the healthy
and diseased retina[ J]. Prog Retin Eye Res, 2006, 25(4): 397-424.
DOI: 10.1016/j.preteyeres.2006.05.003.Bringmann A, Pannicke T, Grosche J, et al. Müller cells in the healthy
and diseased retina[ J]. Prog Retin Eye Res, 2006, 25(4): 397-424.
DOI: 10.1016/j.preteyeres.2006.05.003.
17、Bringmann A, Pannicke T, Biedermann B, et al. Role of retinal glial cells
in neurotransmitter uptake and metabolism[ J]. NeurochemInt, 2009,
54(3-4): 143-160. DOI: 10.1016/j.neuint.2008.10.014.Bringmann A, Pannicke T, Biedermann B, et al. Role of retinal glial cells
in neurotransmitter uptake and metabolism[ J]. NeurochemInt, 2009,
54(3-4): 143-160. DOI: 10.1016/j.neuint.2008.10.014.
18、Reichenbach A, Bringmann A. New functions of Müller cells[ J]. Glia,
2013, 61(5): 651-678. DOI: 10.1002/glia.22477.Reichenbach A, Bringmann A. New functions of Müller cells[ J]. Glia,
2013, 61(5): 651-678. DOI: 10.1002/glia.22477.
19、Xia YF, Li YD, Li X , et al . Identification of alternatively
spliced Act1 and implications for its roles in oncogenesis[ J].
BiochemBiophysResCommun, 2002, 296(2): 406-412. DOI: 10.1016/
s0006-291x(02)00887-2.Xia YF, Li YD, Li X , et al . Identification of alternatively
spliced Act1 and implications for its roles in oncogenesis[ J].
BiochemBiophysResCommun, 2002, 296(2): 406-412. DOI: 10.1016/
s0006-291x(02)00887-2.
20、Novatchkova M, Leibbrandt A, Werzowa J, et al. The STIR-domain
superfamily in signal transduction, development and immunity[ J].
Trends BiochemSci, 2003, 28(5): 226-229. DOI: 10.1016/S0968-
0004(03)00067-7.Novatchkova M, Leibbrandt A, Werzowa J, et al. The STIR-domain
superfamily in signal transduction, development and immunity[ J].
Trends BiochemSci, 2003, 28(5): 226-229. DOI: 10.1016/S0968-
0004(03)00067-7.
21、Hernández-Ramírez E, Sánchez-Chávez G, Estrella-Salazar LA, et al.
Nitrosative stress in the rat retina at the onset of streptozotocin-induced
diabetes[ J]. CellPhysiolBiochem, 2017, 42(6): 2353-2363. DOI:
10.1159/000480007.Hernández-Ramírez E, Sánchez-Chávez G, Estrella-Salazar LA, et al.
Nitrosative stress in the rat retina at the onset of streptozotocin-induced
diabetes[ J]. CellPhysiolBiochem, 2017, 42(6): 2353-2363. DOI:
10.1159/000480007.
22、Carpi-Santos R, de Melo Reis RA, Gomes FCA, et al. Contribution
of Müller cells in the diabetic retinopathy development: focus on
oxidative stress and inflammation[ J]. Antioxidants, 2022, 11(4): 617.
DOI: 10.3390/antiox11040617.Carpi-Santos R, de Melo Reis RA, Gomes FCA, et al. Contribution
of Müller cells in the diabetic retinopathy development: focus on
oxidative stress and inflammation[ J]. Antioxidants, 2022, 11(4): 617.
DOI: 10.3390/antiox11040617.
23、Wang J, Xu X, Elliott MH, et al. Müller cell-derived VEGF is essential
for diabetes-induced retinal inflammation and vascular leakage[ J].
Diabetes, 2010, 59(9): 2297-2305. DOI: 10.2337/db09-1420.Wang J, Xu X, Elliott MH, et al. Müller cell-derived VEGF is essential
for diabetes-induced retinal inflammation and vascular leakage[ J].
Diabetes, 2010, 59(9): 2297-2305. DOI: 10.2337/db09-1420.
24、Penn JS, Madan A, Caldwell RB, et al. Vascular endothelial growth factor
in eye disease[ J]. Prog Retin Eye Res, 2008, 27(4): 331-371. DOI:
10.1016/j.preteyeres.2008.05.001.Penn JS, Madan A, Caldwell RB, et al. Vascular endothelial growth factor
in eye disease[ J]. Prog Retin Eye Res, 2008, 27(4): 331-371. DOI:
10.1016/j.preteyeres.2008.05.001.
25、Bai Y, Ma JX, Guo J, et al. Müller cell-derived VEGF is a significant
contributor to retinal neovascularization[ J]. J Pathol, 2009, 219(4):
446-454. DOI: 10.1002/path.2611.Bai Y, Ma JX, Guo J, et al. Müller cell-derived VEGF is a significant
contributor to retinal neovascularization[ J]. J Pathol, 2009, 219(4):
446-454. DOI: 10.1002/path.2611.
26、Bringmann A, Wiedemann P. Müller glial cells in retinal disease[ J].
O p ht ha l m o l J Int D' o p hta l m o l o g i e Int J O p ht ha l m o l Z Fu r
Augenheilkunde, 2012, 227(1): 1-19. DOI: 10.1159/000328979.Bringmann A, Wiedemann P. Müller glial cells in retinal disease[ J].
O p ht ha l m o l J Int D' o p hta l m o l o g i e Int J O p ht ha l m o l Z Fu r
Augenheilkunde, 2012, 227(1): 1-19. DOI: 10.1159/000328979.
27、Coughlin BA , Feenstra DJ, Mohr S. Müller cells and diabetic
retinopathy[ J]. Vision Res, 2017, 139: 93-100. DOI: 10.1016/
j.visres.2017.03.013.Coughlin BA , Feenstra DJ, Mohr S. Müller cells and diabetic
retinopathy[ J]. Vision Res, 2017, 139: 93-100. DOI: 10.1016/
j.visres.2017.03.013.
28、Vujosevic S, Simó R. Local and systemic inflammatory biomarkers of
diabetic retinopathy: an integrative approach[ J]. Invest Ophthalmol
Vis Sci, 2017, 58(6): BIO68-BIO75. DOI: 10.1167/iovs.17-21769.Vujosevic S, Simó R. Local and systemic inflammatory biomarkers of
diabetic retinopathy: an integrative approach[ J]. Invest Ophthalmol
Vis Sci, 2017, 58(6): BIO68-BIO75. DOI: 10.1167/iovs.17-21769.
29、Liu H, Lessieur EM, Saadane A, et al. Neutrophil elastase contributes
to the pathological vascular permeability characteristic of diabetic
retinopathy[ J]. Diabetologia, 2019, 62(12): 2365-2374. DOI:
10.1007/s00125-019-04998-4.Liu H, Lessieur EM, Saadane A, et al. Neutrophil elastase contributes
to the pathological vascular permeability characteristic of diabetic
retinopathy[ J]. Diabetologia, 2019, 62(12): 2365-2374. DOI:
10.1007/s00125-019-04998-4.
30、Bringmann A, Wiedemann P. Involvement of Müller glial cells in
epiretinal membrane formation[ J]. Graefe's Arch Clin Exp Ophthalmol,
2009, 247(7): 865-883. DOI: 10.1007/s00417-009-1082-x.Bringmann A, Wiedemann P. Involvement of Müller glial cells in
epiretinal membrane formation[ J]. Graefe's Arch Clin Exp Ophthalmol,
2009, 247(7): 865-883. DOI: 10.1007/s00417-009-1082-x.
31、Miossec P, Kolls JK. Targeting IL-17 and TH17 cells in chronic
inflammation[ J]. Nat Rev Drug Discov, 2012, 11(10): 763-776. DOI:
10.1038/nrd3794.Miossec P, Kolls JK. Targeting IL-17 and TH17 cells in chronic
inflammation[ J]. Nat Rev Drug Discov, 2012, 11(10): 763-776. DOI:
10.1038/nrd3794.
32、Mills KHG. IL-17 and IL-17-producing cells in protection versus
pathology[ J]. NatRevImmunol, 2023, 23(1): 38-54. DOI: 10.1038/
s41577-022-00746-9.Mills KHG. IL-17 and IL-17-producing cells in protection versus
pathology[ J]. NatRevImmunol, 2023, 23(1): 38-54. DOI: 10.1038/
s41577-022-00746-9.
33、Shao L, Feng B, Zhang Y, et al. The role of adipose-derived
inflammatory cytokines in type 1 diabetes[ J]. Adipocyte, 2016, 5(3):
270-274. DOI: 10.1080/21623945.2016.1162358.Shao L, Feng B, Zhang Y, et al. The role of adipose-derived
inflammatory cytokines in type 1 diabetes[ J]. Adipocyte, 2016, 5(3):
270-274. DOI: 10.1080/21623945.2016.1162358.
34、Lindstrom SI, Sigurdardottir S, Zapadka TE, et al. Diabetes induces IL-
17A-Act1-FADD-dependent retinal endothelial cell death and capillary
degeneration[ J]. J Diabetes Complications, 2019, 33(9): 668-674.
DOI: 10.1016/j.jdiacomp.2019.05.016.Lindstrom SI, Sigurdardottir S, Zapadka TE, et al. Diabetes induces IL-
17A-Act1-FADD-dependent retinal endothelial cell death and capillary
degeneration[ J]. J Diabetes Complications, 2019, 33(9): 668-674.
DOI: 10.1016/j.jdiacomp.2019.05.016.
35、Chen Y, Yang P, Li F, et al. The effects of Th17 cytokines on the
inflammatory mediator production and barrier function of ARPE-
19 cells[ J]. PLoS One, 2011, 6(3): e18139. DOI: 10.1371/journal.
pone.0018139.Chen Y, Yang P, Li F, et al. The effects of Th17 cytokines on the
inflammatory mediator production and barrier function of ARPE-
19 cells[ J]. PLoS One, 2011, 6(3): e18139. DOI: 10.1371/journal.
pone.0018139.
36、Yan A, Zhang Y, Wang X, et al. Interleukin 35 regulates interleukin
17 expression and T helper 17 in patients with proliferative diabetic
retinopathy[ J]. Bioengineered, 2022, 13(5): 13293-13299. DOI:
10.1080/21655979.2022.2080367.Yan A, Zhang Y, Wang X, et al. Interleukin 35 regulates interleukin
17 expression and T helper 17 in patients with proliferative diabetic
retinopathy[ J]. Bioengineered, 2022, 13(5): 13293-13299. DOI:
10.1080/21655979.2022.2080367.
37、Sigurdardottir S, Zapadka TE, Lindstrom SI, et al. Diabetes-mediated
IL-17A enhances retinal inflammation, oxidative stress, and vascular
permeability[ J]. CellImmunol, 2019, 341: 103921. DOI: 10.1016/
j.cellimm.2019.04.009.Sigurdardottir S, Zapadka TE, Lindstrom SI, et al. Diabetes-mediated
IL-17A enhances retinal inflammation, oxidative stress, and vascular
permeability[ J]. CellImmunol, 2019, 341: 103921. DOI: 10.1016/
j.cellimm.2019.04.009.
38、Qiu AW, Liu QH, Wang JL. Blocking IL-17A Alleviates Diabetic
Retinopathy in Rodents. Cell Physiol Biochem. 2017;41(3):960-972.
doi: 10.1159/000460514.Qiu AW, Liu QH, Wang JL. Blocking IL-17A Alleviates Diabetic
Retinopathy in Rodents. Cell Physiol Biochem. 2017;41(3):960-972.
doi: 10.1159/000460514.
39、Qiu AW, Huang DR, LI B, et al. IL-17A injury to retinal ganglion cells is
mediated by retinal Müller cells in diabetic retinopathy [ J]. Cell Death
Dis, 2021, 12(11): 1057.DOI: 10.1038/s41419-021-04350-y.Qiu AW, Huang DR, LI B, et al. IL-17A injury to retinal ganglion cells is
mediated by retinal Müller cells in diabetic retinopathy [ J]. Cell Death
Dis, 2021, 12(11): 1057.DOI: 10.1038/s41419-021-04350-y.
40、Isailovic N, Daigo K, Mantovani A, et al. Interleukin-17 and innate
immunity in infections and chronic inflammation[ J]. J Autoimmun,
2015, 60: 1-11. DOI: 10.1016/j.jaut.2015.04.006.Isailovic N, Daigo K, Mantovani A, et al. Interleukin-17 and innate
immunity in infections and chronic inflammation[ J]. J Autoimmun,
2015, 60: 1-11. DOI: 10.1016/j.jaut.2015.04.006.
41、Xiao Y, Jin J, Chang M, et al. TPL2 mediates autoimmune inflammation
through activation of the TAK1 axis of IL-17 signaling[ J]. JExp Med,
2014, 211(8): 1689-1702. DOI: 10.1084/jem.20132640.Xiao Y, Jin J, Chang M, et al. TPL2 mediates autoimmune inflammation
through activation of the TAK1 axis of IL-17 signaling[ J]. JExp Med,
2014, 211(8): 1689-1702. DOI: 10.1084/jem.20132640.
42、Rübsam A, Parikh S, Fort PE. Role of inflammation in diabetic
retinopathy[ J]. Int JMol Sci, 2018, 19(4): E942. DOI: 10.3390/
ijms19040942.Rübsam A, Parikh S, Fort PE. Role of inflammation in diabetic
retinopathy[ J]. Int JMol Sci, 2018, 19(4): E942. DOI: 10.3390/
ijms19040942.
43、Xie B, Jiao Q, Cheng Y, et al. Effect of pigment epithelium-derived
factor on glutamate uptake in retinal Muller cells under high-glucose
conditions[ J]. Invest Ophthalmol VisSci, 2012, 53(2): 1023-1032.
DOI: 10.1167/iovs.11-8695.Xie B, Jiao Q, Cheng Y, et al. Effect of pigment epithelium-derived
factor on glutamate uptake in retinal Muller cells under high-glucose
conditions[ J]. Invest Ophthalmol VisSci, 2012, 53(2): 1023-1032.
DOI: 10.1167/iovs.11-8695.
44、Shen X, Xie B, Cheng Y, et al. Effect of pigment epithelium derived
factor on the expression of glutamine synthetase in early phase of
experimental diabetic retinopathy[ J]. Ocul Immunol Inflamm, 2011,
19(4): 246-254. DOI: 10.3109/09273948.2011.580073.Shen X, Xie B, Cheng Y, et al. Effect of pigment epithelium derived
factor on the expression of glutamine synthetase in early phase of
experimental diabetic retinopathy[ J]. Ocul Immunol Inflamm, 2011,
19(4): 246-254. DOI: 10.3109/09273948.2011.580073.
45、Fu S, Dong S, Zhu M, et al. Müller glia are a major cellular source of
survival signals for retinal neurons in diabetes[ J]. Diabetes, 2015,
64(10): 3554-3563. DOI: 10.2337/db15-0180.Fu S, Dong S, Zhu M, et al. Müller glia are a major cellular source of
survival signals for retinal neurons in diabetes[ J]. Diabetes, 2015,
64(10): 3554-3563. DOI: 10.2337/db15-0180.
46、Pathak JL, Fang Y, Chen Y, et al. Downregulation of macrophage�specific act-1 intensifies periodontitis and alveolar bone loss possibly
via TNF/NF-κB signaling[ J]. Front Cell Dev Biol, 2021, 9: 628139.
DOI: 10.3389/fcell.2021.628139.Pathak JL, Fang Y, Chen Y, et al. Downregulation of macrophage�specific act-1 intensifies periodontitis and alveolar bone loss possibly
via TNF/NF-κB signaling[ J]. Front Cell Dev Biol, 2021, 9: 628139.
DOI: 10.3389/fcell.2021.628139.
47、Song X, Qian Y. The activation and regulation of IL-17 receptor
mediated signaling[ J]. Cytokine, 2013, 62(2): 175-182. DOI:
10.1016/j.cyto.2013.03.014.Song X, Qian Y. The activation and regulation of IL-17 receptor
mediated signaling[ J]. Cytokine, 2013, 62(2): 175-182. DOI:
10.1016/j.cyto.2013.03.014.
48、Liu C, Qian W, Qian Y, et al. Act1, a U-box E3 ubiquitin ligase for
IL-17 signaling[ J]. Sci Signal, 2009, 2(92): ra63. DOI: 10.1126/
scisignal.2000382.Liu C, Qian W, Qian Y, et al. Act1, a U-box E3 ubiquitin ligase for
IL-17 signaling[ J]. Sci Signal, 2009, 2(92): ra63. DOI: 10.1126/
scisignal.2000382.
49、Wang Y, Yu H, Li J, et al. Th22 cells induce Müller cell activation via
the Act1/TRAF6 pathway in diabetic retinopathy[ J]. Cell Tissue Res,
2022, 390(3): 367-383. DOI: 10.1007/s00441-022-03689-8.Wang Y, Yu H, Li J, et al. Th22 cells induce Müller cell activation via
the Act1/TRAF6 pathway in diabetic retinopathy[ J]. Cell Tissue Res,
2022, 390(3): 367-383. DOI: 10.1007/s00441-022-03689-8.
50、Wu H, Arron JR . TRAF6, a molecular bridge spanning adaptive
immunity, innate immunity and osteoimmunology[ J]. Bioessays, 2003,
25(11): 1096-1105. DOI: 10.1002/bies.10352.Wu H, Arron JR . TRAF6, a molecular bridge spanning adaptive
immunity, innate immunity and osteoimmunology[ J]. Bioessays, 2003,
25(11): 1096-1105. DOI: 10.1002/bies.10352.
51、WALSH M C, LEE J, CHOI Y. Tumor necrosis factor receptor�associated factor 6 (TRAF6) regulation of development, function,
and homeostasis of the immune system. Immunological reviews 2015,
266(1): 72-92. DOI: 10.1111/imr.12302.WALSH M C, LEE J, CHOI Y. Tumor necrosis factor receptor�associated factor 6 (TRAF6) regulation of development, function,
and homeostasis of the immune system. Immunological reviews 2015,
266(1): 72-92. DOI: 10.1111/imr.12302.
52、Chang SH, Park H, Dong C. Act1 adaptor protein is an immediate
and essential signaling component of interleukin-17 receptor[ J].
J Biol Chem, 2006, 281(47): 35603-35607. DOI: 10.1074/jbc.
C600256200.Chang SH, Park H, Dong C. Act1 adaptor protein is an immediate
and essential signaling component of interleukin-17 receptor[ J].
J Biol Chem, 2006, 281(47): 35603-35607. DOI: 10.1074/jbc.
C600256200.
53、Schwandner R, Yamaguchi K, Cao Z. Requirement of tumor necrosis
factor receptor-associated factor (TRAF)6 in interleukin 17 signal
transduction[ J]. J Exp Med, 2000, 191(7): 1233-1240. DOI: 10.1084/
jem.191.7.1233.Schwandner R, Yamaguchi K, Cao Z. Requirement of tumor necrosis
factor receptor-associated factor (TRAF)6 in interleukin 17 signal
transduction[ J]. J Exp Med, 2000, 191(7): 1233-1240. DOI: 10.1084/
jem.191.7.1233.
54、Kanamori M, Kai C, Hayashizaki Y, et al. NF-kappa B activator Act1
associates with IL-1/Toll pathway adaptor molecule TRAF6[ J]. FEBS
Lett, 2002, 532(1-2): 241-246. DOI: 10.1016/s0014-5793(02)03688-8.Kanamori M, Kai C, Hayashizaki Y, et al. NF-kappa B activator Act1
associates with IL-1/Toll pathway adaptor molecule TRAF6[ J]. FEBS
Lett, 2002, 532(1-2): 241-246. DOI: 10.1016/s0014-5793(02)03688-8.
55、Bradley JR, Pober JS. Tumor necrosis factor receptor-associated factors
(TRAFs)[ J]. Oncogene, 2001, 20(44): 6482-6491. DOI: 10.1038/
sj.onc.1204788.Bradley JR, Pober JS. Tumor necrosis factor receptor-associated factors
(TRAFs)[ J]. Oncogene, 2001, 20(44): 6482-6491. DOI: 10.1038/
sj.onc.1204788.
56、Vos S, Aaron R, Weng M, et al. CD40 upregulation in the retina of
patients with diabetic retinopathy: association with TRAF2/TRAF6
upregulation and inflammatory molecule expression[ J]. Invest
Ophthalmol Vis Sci, 2023, 64(7): 17. DOI: 10.1167/iovs.64.7.17.Vos S, Aaron R, Weng M, et al. CD40 upregulation in the retina of
patients with diabetic retinopathy: association with TRAF2/TRAF6
upregulation and inflammatory molecule expression[ J]. Invest
Ophthalmol Vis Sci, 2023, 64(7): 17. DOI: 10.1167/iovs.64.7.17.
57、Kobayashi T, WalshMC, Choi Y. The role of TRAF6 in signal
transduction and the immune response[ J]. Microbes Infect, 2004,
6(14): 1333-1338. DOI: 10.1016/j.micinf.2004.09.001.Kobayashi T, WalshMC, Choi Y. The role of TRAF6 in signal
transduction and the immune response[ J]. Microbes Infect, 2004,
6(14): 1333-1338. DOI: 10.1016/j.micinf.2004.09.001.
58、Tak PP, Firestein GS. NF-kappa B: a key role in inflammatory
diseases[ J]. J ClinInvest, 2001, 107(1): 7-11. DOI: 10.1172/JCI11830.Tak PP, Firestein GS. NF-kappa B: a key role in inflammatory
diseases[ J]. J ClinInvest, 2001, 107(1): 7-11. DOI: 10.1172/JCI11830.
59、Li Q, Verma IM. NF-kappaB regulation in the immune system[ J].
Nat Rev Immunol, 2002, 2(10): 725-734. DOI: 10.1038/nri910.Li Q, Verma IM. NF-kappaB regulation in the immune system[ J].
Nat Rev Immunol, 2002, 2(10): 725-734. DOI: 10.1038/nri910.
60、Karin M, Ben-Neriah Y. Phosphorylation meets ubiquitination: the
control of NF-[kappa]B activity[ J]. Annu Rev Immunol, 2000, 18: 621-
663. DOI: 10.1146/annurev.immunol.18.1.621.Karin M, Ben-Neriah Y. Phosphorylation meets ubiquitination: the
control of NF-[kappa]B activity[ J]. Annu Rev Immunol, 2000, 18: 621-
663. DOI: 10.1146/annurev.immunol.18.1.621.
61、Almalki WH, Almujri SS. The impact of NF-κB on inflammatory and
angiogenic processes in age-related macular degeneration[ J]. ExpEye
Res, 2024, 248: 110111. DOI: 10.1016/j.exer.2024.110111.Almalki WH, Almujri SS. The impact of NF-κB on inflammatory and
angiogenic processes in age-related macular degeneration[ J]. ExpEye
Res, 2024, 248: 110111. DOI: 10.1016/j.exer.2024.110111.
62、Li J, Chen K, Li X, et al. Mechanistic insights into the alterations and
regulation of the AKT signaling pathway in diabetic retinopathy[ J].
Cell Death Discov, 2023, 9(1): 418. DOI: 10.1038/s41420-023-01717-
2.Li J, Chen K, Li X, et al. Mechanistic insights into the alterations and
regulation of the AKT signaling pathway in diabetic retinopathy[ J].
Cell Death Discov, 2023, 9(1): 418. DOI: 10.1038/s41420-023-01717-
2.
63、Ding Y, Chen L, Xu J, et al. NR2E3 inhibits the inflammation and
apoptosis in diabetic retinopathy by regulating the AHR/IL-17A
signaling pathway[ J]. Naunyn Schmiedebergs Arch Pharmacol, 2024: 9081-9094. DOI: 10.1007/s00210-024-03213-5.Ding Y, Chen L, Xu J, et al. NR2E3 inhibits the inflammation and
apoptosis in diabetic retinopathy by regulating the AHR/IL-17A
signaling pathway[ J]. Naunyn Schmiedebergs Arch Pharmacol, 2024: 9081-9094. DOI: 10.1007/s00210-024-03213-5.
64、Li X , Qin W, Qin X , et al. Meta-analysis of the relationship
bet ween ocular and per ipheral ser um IL -17A and diabetic
retinopathy[ J]. Front Endocrinol, 2024, 15: 1320632. DOI: 10.3389/
fendo.2024.1320632.Li X , Qin W, Qin X , et al. Meta-analysis of the relationship
bet ween ocular and per ipheral ser um IL -17A and diabetic
retinopathy[ J]. Front Endocrinol, 2024, 15: 1320632. DOI: 10.3389/
fendo.2024.1320632.
65、Zhou AY, Taylor BE, Barber KG, et al. Anti-IL17A halts the onset of
diabetic retinopathy in type I and II diabetic mice[ J]. Int JMol Sci, 2023,
24(2): 1347. DOI: 10.3390/ijms24021347.Zhou AY, Taylor BE, Barber KG, et al. Anti-IL17A halts the onset of
diabetic retinopathy in type I and II diabetic mice[ J]. Int JMol Sci, 2023,
24(2): 1347. DOI: 10.3390/ijms24021347.
66、Giuliari GP. Diabetic retinopathy: current and new treatment
options[ J ]. Curr Diabetes Rev, 2012, 8(1) : 32-41. DOI :
10.2174/157339912798829188.Giuliari GP. Diabetic retinopathy: current and new treatment
options[ J ]. Curr Diabetes Rev, 2012, 8(1) : 32-41. DOI :
10.2174/157339912798829188.