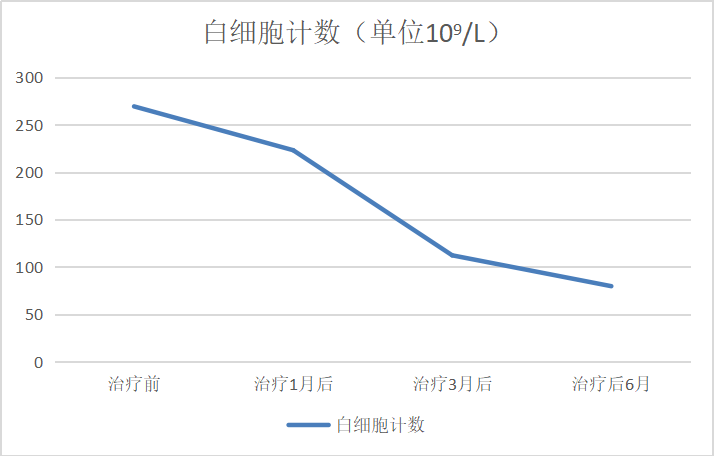
急性泪囊炎常由慢性泪囊炎急性发作引发,典型症状为流泪,异常分泌物增多等慢性泪囊炎症状,继发泪囊区红肿热痛等急性泪囊炎表现,多为单眼发病。慢性淋巴细胞白血病(chronic lymphocytic leukemia, CLL)属于原发于造血组织的恶性血液疾病,从表面看这两种疾病在病理生理方面没有直接联系。本研究报告了1例以急性泪囊炎作为首发症状的CLL患者,表现为双眼急性泪囊炎体征,经全身检查确诊为CLL。同时,通过回顾相关文献,发现有类似报道,但一例为小儿白血病患者以急性泪囊炎首发体征出现,一例急性泪囊炎患者泪囊摘除后经病理活检确诊为CLL,目前尚未见关于CLL保守治疗后急性泪囊炎明显缓解的报道。该病的发生可能与泪道引流相关淋巴组织(lacrimal drainage-associated lymphoid tissue, LDALT)改变有关,它作为黏膜免疫系统的一部分,可引导CLL细胞向LDALT迁移并定植,破坏局部的免疫微环境,干扰泪道的免疫平衡,抑制正常免疫细胞的功能,促进鼻泪管淋巴细胞异常增生等,引发泪道系统引流不畅。同时,此外,CLL所致的全身免疫抑制状态,也使得机体整体抗感染能力降低,增加了泪囊感染的风险,最终导致急性泪囊炎的发生和发展。通过对该病例的潜在发病机制进行综合分析,并探讨其为临床诊疗带来的启示。
Acute dacryocystitis often results from the acute attack exacerbation of chronic dacryocystitis. Typical symptoms include those of chronic dacryocystitis, such as persistent tearing, increased abnormal secretions, as well secondary manifestations of acute dacryocystitis like redness, swelling, heat and pain in the lacrimal sac area, which are predominantly unilateral. Chronic lymphocytic leukemia (CLL) is a malignant blood disorder originating from hematopoietic tissue. On the surface, these two diseases do not appear to be directly related in terms of pathophysiology. This study reported a case of CLL presenting with acute dacryocystitis as the initial symptom. The patient exhibited signs of acute dacryocystitis in both eyes, and was subsequently diagnosed with CLL following a systemic examination. Meanwhile, a review of the relevant literature revealed similar reports. However, in one instance, acute dacryocystitis in children with leukemia appeared as the first sign of acute leukemia itself, while in another, acute dacryocystitis was diagnosed as CLL by pathological biopsy after dacryocystectomy. At present, there have been no report of significant remission of acute dacryocystitis following conservative treatment for CLL. The occurrence of this condition may be related to the changes in lacrimal drainage-associated lymphoid tissue (LDALT). As a part of the mucosal immune system, LDALT can guide CLL cells to migrate and colonize within it, thereby disrupting the local immune microenvironment, interfering with the immune balance of the lacrimal passage, inhibiting the function of normal immune cells, promoting abnormal lymphocyte proliferation in the nasolacrimal duct, and ultimately leading to impaired drainage of the lacrimal passage system. Additionally, the systemic immunosuppressive state induced by CLL reduces the body’s overall anti-infective capacity, increasing the risk of dacryocystal infection and ultimately contributing to the onset and progression of acute dacryocystitis. Through a comprehensive analysis of the potential pathogenesis of this case, we aim to explore its implications for clinical diagnosis and treatment.