1、Willvonseder R, Goldstein NP, McCall JT, et al. A hereditary disorder
with dementia, spastic dysarthria, vertical eye movement paresis, gait
disturbance, splenomegaly, and abnormal copper metabolism[ J].
Neurology, 1973, 23(10): 1039-1049.Willvonseder R, Goldstein NP, McCall JT, et al. A hereditary disorder
with dementia, spastic dysarthria, vertical eye movement paresis, gait
disturbance, splenomegaly, and abnormal copper metabolism[ J].
Neurology, 1973, 23(10): 1039-1049.
2、Dix MR. Clinical observations upon the vestibular responses in certain
disorders of the central nervous system[ J]. Adv Otorhinolaryngol,
1970, 17: 118-128.Dix MR. Clinical observations upon the vestibular responses in certain
disorders of the central nervous system[ J]. Adv Otorhinolaryngol,
1970, 17: 118-128.
3、贾建平, 陈生第. 神经病学[M]. 第8版. 北京: 人民卫生出版社, 2013.
JIA JP, CHEN SD. Neurology[M]. 8th ed. Beijing: People’s
Medical Publishing House, 2013.贾建平, 陈生第. 神经病学[M]. 第8版. 北京: 人民卫生出版社, 2013.
JIA JP, CHEN SD. Neurology[M]. 8th ed. Beijing: People’s
Medical Publishing House, 2013.
4、Bayne T, Brainard D, Byrne RW, et al. What is cognition[ J]. Curr Biol,
2019, 29(13): R608-R615.Bayne T, Brainard D, Byrne RW, et al. What is cognition[ J]. Curr Biol,
2019, 29(13): R608-R615.
5、Petersen RC. Mild cognitive impairment as a diagnostic entity[ J]. J
Intern Med, 2004, 256(3): 183-194.Petersen RC. Mild cognitive impairment as a diagnostic entity[ J]. J
Intern Med, 2004, 256(3): 183-194.
6、Hill NT, Mowszowski L, Naismith SL, et al. Computerized cognitive
training in older adults with mild cognitive impairment or dementia: a
systematic review and meta-analysis[ J]. Am J Psychiatry, 2017, 174(4):
329-340.Hill NT, Mowszowski L, Naismith SL, et al. Computerized cognitive
training in older adults with mild cognitive impairment or dementia: a
systematic review and meta-analysis[ J]. Am J Psychiatry, 2017, 174(4):
329-340.
7、Martin M, Clare L, Altgassen AM, et al. Cognition‐based interventions
for healthy older people and people with mild cognitive impairment[ J].
Cochrane Database Syst Rev, 2011(1): CD006220.Martin M, Clare L, Altgassen AM, et al. Cognition‐based interventions
for healthy older people and people with mild cognitive impairment[ J].
Cochrane Database Syst Rev, 2011(1): CD006220.
8、Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and management of
dementia: review[ J]. JAMA, 2019, 322(16): 1589-1599.Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and management of
dementia: review[ J]. JAMA, 2019, 322(16): 1589-1599.
9、Lane CA, Hardy J, Schott JM. Alzheimer’s disease[ J]. Eur J Neurol
2018, 25(1): 59-70.Lane CA, Hardy J, Schott JM. Alzheimer’s disease[ J]. Eur J Neurol
2018, 25(1): 59-70.
10、Prince MJ. World Alzheimer Report 2015: the global impact of
dementia: an analysis of prevalence, incidence, cost and trends:
Alzheimer’s Disease International[R]. London: Alzheimer’s Disease
International, 2015.Prince MJ. World Alzheimer Report 2015: the global impact of
dementia: an analysis of prevalence, incidence, cost and trends:
Alzheimer’s Disease International[R]. London: Alzheimer’s Disease
International, 2015.
11、Xu J, Wang J, Wimo A, et al. The economic burden of dementia in
China, 1990–2030: implications for health policy[ J]. Bull World
Health Organ, 2017, 95(1): 18.Xu J, Wang J, Wimo A, et al. The economic burden of dementia in
China, 1990–2030: implications for health policy[ J]. Bull World
Health Organ, 2017, 95(1): 18.
12、Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention,
intervention, and care[ J]. Lancet, 2017, 390(10113): 2673-2734.Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention,
intervention, and care[ J]. Lancet, 2017, 390(10113): 2673-2734.
13、Petersen RC, Morris JC. Mild cognitive impairment as a clinical entity
and treatment target[ J]. Arch Neurol, 2005, 62(7): 1160-1163.Petersen RC, Morris JC. Mild cognitive impairment as a clinical entity
and treatment target[ J]. Arch Neurol, 2005, 62(7): 1160-1163.
14、Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment--
beyond controversies, towards a consensus: report of the International
Working Group on Mild Cognitive Impairment[ J]. J Intern Med, 2004,
256(3): 240-246.Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment--
beyond controversies, towards a consensus: report of the International
Working Group on Mild Cognitive Impairment[ J]. J Intern Med, 2004,
256(3): 240-246.
15、Harper L, Barkhof F, Scheltens P, et al. An algorithmic approach to
structural imaging in dementia[ J]. J Neurol Neurosurg Psychiatry,
2014, 85(6): 692-698.Harper L, Barkhof F, Scheltens P, et al. An algorithmic approach to
structural imaging in dementia[ J]. J Neurol Neurosurg Psychiatry,
2014, 85(6): 692-698.
16、Duara R, Loewenstein DA, Potter E, et al. Medial temporal lobe atrophy
on MRI scans and the diagnosis of Alzheimer disease[ J]. Neurology,
2008, 71(24): 1986-1992.Duara R, Loewenstein DA, Potter E, et al. Medial temporal lobe atrophy
on MRI scans and the diagnosis of Alzheimer disease[ J]. Neurology,
2008, 71(24): 1986-1992.
17、Burton EJ, Barber R, Mukaetova-Ladinska EB, et al. Medial temporal
lobe atrophy on MRI differentiates Alzheimer’s disease from dementia
with Lewy bodies and vascular cognitive impairment: a prospective
study with pathological verification of diagnosis[ J]. Brain, 2009,
132(Pt 1): 195-203.Burton EJ, Barber R, Mukaetova-Ladinska EB, et al. Medial temporal
lobe atrophy on MRI differentiates Alzheimer’s disease from dementia
with Lewy bodies and vascular cognitive impairment: a prospective
study with pathological verification of diagnosis[ J]. Brain, 2009,
132(Pt 1): 195-203.
18、Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter:
diagnosis of dementia (an evidence-based review). Report of the
Quality Standards Subcommittee of the American Academy of
Neurology[ J]. Neurology, 2001, 56(9): 1143-1153.Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter:
diagnosis of dementia (an evidence-based review). Report of the
Quality Standards Subcommittee of the American Academy of
Neurology[ J]. Neurology, 2001, 56(9): 1143-1153.
19、Anderson TJ, MacAskill MR . Eye movements in patients with
neurodegenerative disorders[ J]. Nat Rev Neurol, 2013, 9(2): 74-85.Anderson TJ, MacAskill MR . Eye movements in patients with
neurodegenerative disorders[ J]. Nat Rev Neurol, 2013, 9(2): 74-85.
20、Bridgeman B. Conscious vs unconscious processes: the case of
vision[ J]. Theory Psychol, 1992, 2(1): 73-88.Bridgeman B. Conscious vs unconscious processes: the case of
vision[ J]. Theory Psychol, 1992, 2(1): 73-88.
21、Deubel H, Schneider WX. Delayed saccades, but not delayed manual
aiming movements, require visual attention shifts[ J]. Ann N Y Acad
Sci, 2003, 1004(1): 289-296.Deubel H, Schneider WX. Delayed saccades, but not delayed manual
aiming movements, require visual attention shifts[ J]. Ann N Y Acad
Sci, 2003, 1004(1): 289-296.
22、Girard B, Berthoz A. From brainstem to cortex: computational
models of saccade generation circuitry[ J]. Prog Neurobiol, 2005,
77(4): 215-251.Girard B, Berthoz A. From brainstem to cortex: computational
models of saccade generation circuitry[ J]. Prog Neurobiol, 2005,
77(4): 215-251.
23、Pierrot-Deseilligny C, Rivaud S, Gaymard B, et al. Cortical control of
saccades[ J]. Ann Neurol, 1995, 37(5): 557-567.Pierrot-Deseilligny C, Rivaud S, Gaymard B, et al. Cortical control of
saccades[ J]. Ann Neurol, 1995, 37(5): 557-567.
24、Coiner B, Pan H, Bennett ML, et al. Functional neuroanatomy of the
human eye movement network: a review and atlas[ J]. Brain Struct
Funct, 2019, 224(8): 2603-2617.Coiner B, Pan H, Bennett ML, et al. Functional neuroanatomy of the
human eye movement network: a review and atlas[ J]. Brain Struct
Funct, 2019, 224(8): 2603-2617.
25、Stuphorn V, Taylor TL, Schall JD. Performance monitoring by the
supplementary eye field[ J]. Nature, 2000, 408(6814): 857-860.Stuphorn V, Taylor TL, Schall JD. Performance monitoring by the
supplementary eye field[ J]. Nature, 2000, 408(6814): 857-860.
26、Parton A , Nachev P, Hodgson TL, et al. Role of the human
supplementary eye field in the control of saccadic eye movements[ J].
Neuropsychologia, 2007, 45(5): 997-1008.Parton A , Nachev P, Hodgson TL, et al. Role of the human
supplementary eye field in the control of saccadic eye movements[ J].
Neuropsychologia, 2007, 45(5): 997-1008.
27、Quaia C, Lefèvre P, Optican LM. Model of the control of saccades by
superior colliculus and cerebellum[ J]. J Neurophysiol, 1999, 82(2):
999-1018.Quaia C, Lefèvre P, Optican LM. Model of the control of saccades by
superior colliculus and cerebellum[ J]. J Neurophysiol, 1999, 82(2):
999-1018.
28、Pierrot-Deseilligny C, Müri RM, Nyffeler T, et al. The role of the human
dorsolateral prefrontal cortex in ocular motor behavior[ J]. Ann N Y
Acad Sci, 2005, 1039: 239-251.Pierrot-Deseilligny C, Müri RM, Nyffeler T, et al. The role of the human
dorsolateral prefrontal cortex in ocular motor behavior[ J]. Ann N Y
Acad Sci, 2005, 1039: 239-251.
29、Tulunay-Keesey U. Fading of stabilized retinal images[ J]. J Opt Soc
Am, 1982, 72(4): 440-447.Tulunay-Keesey U. Fading of stabilized retinal images[ J]. J Opt Soc
Am, 1982, 72(4): 440-447.
30、Kapoula Z, Yang Q, Otero-Millan J, et al. Distinctive features
of microsaccades in Alzheimer’s disease and in mild cognitive
impairment[ J]. Age, 2014, 36(2): 535-543.Kapoula Z, Yang Q, Otero-Millan J, et al. Distinctive features
of microsaccades in Alzheimer’s disease and in mild cognitive
impairment[ J]. Age, 2014, 36(2): 535-543.
31、Abadi RV, Gowen E. Characteristics of saccadic intrusions[ J]. Vision
Res 2004, 44(23): 2675-2690.Abadi RV, Gowen E. Characteristics of saccadic intrusions[ J]. Vision
Res 2004, 44(23): 2675-2690.
32、Martinez-Conde S. Fixational eye movements in normal and
pathological vision[ J]. Prog Brain Res, 2006, 154: 151-176.Martinez-Conde S. Fixational eye movements in normal and
pathological vision[ J]. Prog Brain Res, 2006, 154: 151-176.
33、Otero-Millan J, Macknik SL, Serra A, et al. Triggering mechanisms in
microsaccade and saccade generation: a novel proposal[ J]. Ann N Y
Acad Sci, 2011, 1233: 107-116.Otero-Millan J, Macknik SL, Serra A, et al. Triggering mechanisms in
microsaccade and saccade generation: a novel proposal[ J]. Ann N Y
Acad Sci, 2011, 1233: 107-116.
34、Martinez-Conde S, Otero-Millan J, Macknik SL. The impact of
microsaccades on vision: towards a unified theory of saccadic
function[ J]. Nat Rev Neurosci, 2013, 14(2): 83-96.Martinez-Conde S, Otero-Millan J, Macknik SL. The impact of
microsaccades on vision: towards a unified theory of saccadic
function[ J]. Nat Rev Neurosci, 2013, 14(2): 83-96.
35、Thier P, Ilg UJ. The neural basis of smooth-pursuit eye movements[ J].
Curr Opin Neurobiol, 2005, 15(6): 645-652.Thier P, Ilg UJ. The neural basis of smooth-pursuit eye movements[ J].
Curr Opin Neurobiol, 2005, 15(6): 645-652.
36、Fukushima K. Frontal cortical control of smooth-pursuit[ J]. Curr Opin
Neurobiol, 2003, 13(6): 647-654.Fukushima K. Frontal cortical control of smooth-pursuit[ J]. Curr Opin
Neurobiol, 2003, 13(6): 647-654.
37、Petit L, Haxby JV. Functional anatomy of pursuit eye movements in
humans as revealed by fMRI[ J]. J Neurophysiol, 1999, 82(1): 463-471.Petit L, Haxby JV. Functional anatomy of pursuit eye movements in
humans as revealed by fMRI[ J]. J Neurophysiol, 1999, 82(1): 463-471.
38、Yan YJ, Cui DM, Lynch JC. Overlap of saccadic and pursuit eye
movement systems in the brain stem reticular formation[ J]. J
Neurophysiol, 2001, 86(6): 3056-3060.Yan YJ, Cui DM, Lynch JC. Overlap of saccadic and pursuit eye
movement systems in the brain stem reticular formation[ J]. J
Neurophysiol, 2001, 86(6): 3056-3060.
39、赵堪兴, 杨培增. 眼科学[M]. 第8版. 北京: 人民卫生出版社,
2013: 23-24.
ZHAO KX, YANG PZ. Ophthalmology[M]. 8th ed. Beijing:
People’s Medical Publishing House, 2013: 23-24.赵堪兴, 杨培增. 眼科学[M]. 第8版. 北京: 人民卫生出版社,
2013: 23-24.
ZHAO KX, YANG PZ. Ophthalmology[M]. 8th ed. Beijing:
People’s Medical Publishing House, 2013: 23-24.
40、Sanford AM. Mild cognitive impairment[ J]. Clin Geriatr Med, 2017,
33(3): 325-337.Sanford AM. Mild cognitive impairment[ J]. Clin Geriatr Med, 2017,
33(3): 325-337.
41、Tschanz JT, Welsh-Bohmer KA, Lyketsos CG, et al. Conversion to
dementia from mild cognitive disorder: the Cache County Study[ J].
Neurology, 2006, 67(2): 229-234.Tschanz JT, Welsh-Bohmer KA, Lyketsos CG, et al. Conversion to
dementia from mild cognitive disorder: the Cache County Study[ J].
Neurology, 2006, 67(2): 229-234.
42、Petersen RC. Mild cognitive impairment: current research and clinical
implications[ J]. Semin Neurol, 2007, 27(1): 22-31.Petersen RC. Mild cognitive impairment: current research and clinical
implications[ J]. Semin Neurol, 2007, 27(1): 22-31.
43、Yang Q, Wang T, Su N, et al. Specific saccade deficits in patients with
Alzheimer’s disease at mild to moderate stage and in patients with
amnestic mild cognitive impairment[ J]. Age, 2013, 35(4): 1287-1298.Yang Q, Wang T, Su N, et al. Specific saccade deficits in patients with
Alzheimer’s disease at mild to moderate stage and in patients with
amnestic mild cognitive impairment[ J]. Age, 2013, 35(4): 1287-1298.
44、Chehrehnegar N, Nejati V, Shati M, et al. Behavioral and cognitive
markers of mild cognitive impairment: diagnostic value of saccadic eye
movements and Simon task[ J]. Aging Clin Exp Res, 2019, 31(11):
1591-1600.Chehrehnegar N, Nejati V, Shati M, et al. Behavioral and cognitive
markers of mild cognitive impairment: diagnostic value of saccadic eye
movements and Simon task[ J]. Aging Clin Exp Res, 2019, 31(11):
1591-1600.
45、Alichniewicz KK, Brunner F, Klünemann HH, et al. Neural correlates
of saccadic inhibition in healthy elderly and patients with amnestic mild
cognitive impairment[ J]. Front Psychol, 2013, 4: 467.Alichniewicz KK, Brunner F, Klünemann HH, et al. Neural correlates
of saccadic inhibition in healthy elderly and patients with amnestic mild
cognitive impairment[ J]. Front Psychol, 2013, 4: 467.
46、Fletcher WA, Sharpe JA. Saccadic eye movement dysfunction in
Alzheimer’s disease[ J]. Ann Neurol, 1986, 20(4): 464-471.Fletcher WA, Sharpe JA. Saccadic eye movement dysfunction in
Alzheimer’s disease[ J]. Ann Neurol, 1986, 20(4): 464-471.
47、Shafiq-Antonacci R, Maruff P, Masters C, et al. Spectrum of saccade
system function in Alzheimer disease[ J]. Arch Neurol, 2003, 60(9):
1272-1278.Shafiq-Antonacci R, Maruff P, Masters C, et al. Spectrum of saccade
system function in Alzheimer disease[ J]. Arch Neurol, 2003, 60(9):
1272-1278.
48、Kahana Levy N, Lavidor M, Vakil E. Prosaccade and antisaccade
paradigms in persons with Alzheimer’s disease: a meta-analytic
review[ J]. Neuropsychol Rev, 2018, 28(1): 16-31.Kahana Levy N, Lavidor M, Vakil E. Prosaccade and antisaccade
paradigms in persons with Alzheimer’s disease: a meta-analytic
review[ J]. Neuropsychol Rev, 2018, 28(1): 16-31.
49、Yang Q, Wang T, Su N, et al. Long latency and high variability in
accuracy-speed of prosaccades in Alzheimer’s disease at mild to
moderate stage[ J]. Dement Geriatr Cogn Dis Extra, 2011, 1(1):
318-329.Yang Q, Wang T, Su N, et al. Long latency and high variability in
accuracy-speed of prosaccades in Alzheimer’s disease at mild to
moderate stage[ J]. Dement Geriatr Cogn Dis Extra, 2011, 1(1):
318-329.
50、Peltsch A, Hemraj A, Garcia A, et al. Saccade deficits in amnestic mild
cognitive impairment resemble mild Alzheimer’s disease[ J]. Eur J
Neurosci, 2014, 39(11): 2000-2013.Peltsch A, Hemraj A, Garcia A, et al. Saccade deficits in amnestic mild
cognitive impairment resemble mild Alzheimer’s disease[ J]. Eur J
Neurosci, 2014, 39(11): 2000-2013.
51、Garbutt S, Matlin A, Hellmuth J, et al. Oculomotor function in
frontotemporal lobar degeneration, related disorders and Alzheimer’s
disease[ J]. Brain, 2008, 131(Pt 5): 1268-1281.Garbutt S, Matlin A, Hellmuth J, et al. Oculomotor function in
frontotemporal lobar degeneration, related disorders and Alzheimer’s
disease[ J]. Brain, 2008, 131(Pt 5): 1268-1281.
52、Posner MI, Petersen SE. The attention system of the human brain[ J].
Annu Rev Neurosci, 1990, 13: 25-42.Posner MI, Petersen SE. The attention system of the human brain[ J].
Annu Rev Neurosci, 1990, 13: 25-42.
53、Kaufman LD, Pratt J, Levine B, et al. Executive deficits detected in mild
Alzheimer’s disease using the antisaccade task[ J]. Brain Behav, 2012,
2(1): 15-21.Kaufman LD, Pratt J, Levine B, et al. Executive deficits detected in mild
Alzheimer’s disease using the antisaccade task[ J]. Brain Behav, 2012,
2(1): 15-21.
54、Crawford TJ, Higham S, Mayes J, et al. The role of working memory
and attentional disengagement on inhibitory control: effects of aging
and Alzheimer’s disease[ J]. Age, 2013, 35(5): 1637-1650.Crawford TJ, Higham S, Mayes J, et al. The role of working memory
and attentional disengagement on inhibitory control: effects of aging
and Alzheimer’s disease[ J]. Age, 2013, 35(5): 1637-1650.
55、Currie J, Ramsden B, McArthur C, et al. Validation of a clinical
antisaccadic eye movement test in the assessment of dementia[ J]. Arch
Neurol, 1991, 48(6): 644-648.Currie J, Ramsden B, McArthur C, et al. Validation of a clinical
antisaccadic eye movement test in the assessment of dementia[ J]. Arch
Neurol, 1991, 48(6): 644-648.
56、Abel LA, Unverzagt F, Yee RD. Effects of stimulus predictability and
interstimulus gap on saccades in Alzheimer’s disease[ J]. Dement
Geriatr Cogn Disord, 2002, 13(4): 235-243.Abel LA, Unverzagt F, Yee RD. Effects of stimulus predictability and
interstimulus gap on saccades in Alzheimer’s disease[ J]. Dement
Geriatr Cogn Disord, 2002, 13(4): 235-243.
57、Heuer HW, Mirsky JB, Kong EL, et al. Antisaccade task reflects cortical
involvement in mild cognitive impairment[ J]. Neurology, 2013,
81(14): 1235-1243.Heuer HW, Mirsky JB, Kong EL, et al. Antisaccade task reflects cortical
involvement in mild cognitive impairment[ J]. Neurology, 2013,
81(14): 1235-1243.
58、Bylsma FW, Rasmusson DX, Rebok GW, et al. Changes in visual
fixation and saccadic eye movements in Alzheimer’s disease[ J]. Int J
Psychophysiol, 1995, 19(1): 33-40.Bylsma FW, Rasmusson DX, Rebok GW, et al. Changes in visual
fixation and saccadic eye movements in Alzheimer’s disease[ J]. Int J
Psychophysiol, 1995, 19(1): 33-40.
59、Boxer AL, Garbutt S, Rankin KP, et al. Medial versus lateral frontal lobe
contributions to voluntary saccade control as revealed by the study of
patients with frontal lobe degeneration[ J]. J Neurosci, 2006, 26(23):
6354-6363.Boxer AL, Garbutt S, Rankin KP, et al. Medial versus lateral frontal lobe
contributions to voluntary saccade control as revealed by the study of
patients with frontal lobe degeneration[ J]. J Neurosci, 2006, 26(23):
6354-6363.
60、Zaccara G, Gangemi PF, Muscas GC, et al. Smooth-pursuit eye
movements: alterations in Alzheimer’s disease[ J]. J Neurol Sci, 1992,
112(1-2): 81-89.Zaccara G, Gangemi PF, Muscas GC, et al. Smooth-pursuit eye
movements: alterations in Alzheimer’s disease[ J]. J Neurol Sci, 1992,
112(1-2): 81-89.
61、Pavisic IM, Firth NC, Parsons S, et al. Eyetracking metrics in young
onset Alzheimer’s disease: a window into cognitive visual functions[ J].
Front Neurol, 2017, 8: 377.Pavisic IM, Firth NC, Parsons S, et al. Eyetracking metrics in young
onset Alzheimer’s disease: a window into cognitive visual functions[ J].
Front Neurol, 2017, 8: 377.
62、Hutton JT, Nagel JA, Loewenson RB. Eye tracking dysfunction in
Alzheimer-type dementia[ J]. Neurology, 1984, 34(1): 99-102.Hutton JT, Nagel JA, Loewenson RB. Eye tracking dysfunction in
Alzheimer-type dementia[ J]. Neurology, 1984, 34(1): 99-102.
63、Moser A, K?mpf D, Olschinka J. Eye movement dysfunction in
dementia of the Alzheimer type[ J]. Dementia, 1995, 6(5): 264-268.Moser A, K?mpf D, Olschinka J. Eye movement dysfunction in
dementia of the Alzheimer type[ J]. Dementia, 1995, 6(5): 264-268.
64、Fotiou DF, Stergiou V, Tsiptsios D, et al. Cholinergic deficiency in
Alzheimer’s and Parkinson’s disease: evaluation with pupillometry[ J].
Int J Psychophysiol, 2009, 73(2): 143-149.Fotiou DF, Stergiou V, Tsiptsios D, et al. Cholinergic deficiency in
Alzheimer’s and Parkinson’s disease: evaluation with pupillometry[ J].
Int J Psychophysiol, 2009, 73(2): 143-149.
65、Fotiou F, Fountoulakis KN, Tsolaki M, et al. Changes in pupil reaction
to light in Alzheimer’s disease patients: a preliminary report[ J]. Int J
Psychophysiol, 2000, 37(1): 111-120.Fotiou F, Fountoulakis KN, Tsolaki M, et al. Changes in pupil reaction
to light in Alzheimer’s disease patients: a preliminary report[ J]. Int J
Psychophysiol, 2000, 37(1): 111-120.
66、Crawford TJ, Higham S, Renvoize T, et al. Inhibitory control of saccadic
eye movements and cognitive impairment in Alzheimer’s disease[ J].
Biol Psychiatry, 2005, 57(9): 1052-1060.Crawford TJ, Higham S, Renvoize T, et al. Inhibitory control of saccadic
eye movements and cognitive impairment in Alzheimer’s disease[ J].
Biol Psychiatry, 2005, 57(9): 1052-1060.
67、LeCun Y, Bengio Y, Hinton G. Deep learning[ J]. Nature, 2015,
521(7553): 436-444.LeCun Y, Bengio Y, Hinton G. Deep learning[ J]. Nature, 2015,
521(7553): 436-444.
68、Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular
risk factors from retinal fundus photographs via deep learning[ J]. Nat
Biomed Eng, 2018, 2(3): 158-164.Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular
risk factors from retinal fundus photographs via deep learning[ J]. Nat
Biomed Eng, 2018, 2(3): 158-164.
69、Long E, Liu Z, Xiang Y, et al. Discrimination of the behavioural
dynamics of visually impaired infants via deep learning[ J]. Nat Biomed
Eng, 2019, 3(11): 860-869.Long E, Liu Z, Xiang Y, et al. Discrimination of the behavioural
dynamics of visually impaired infants via deep learning[ J]. Nat Biomed
Eng, 2019, 3(11): 860-869.
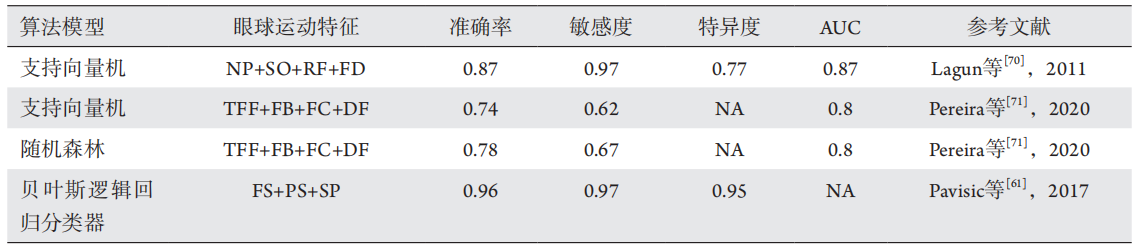
70、Lagun D, Manzanares C, Zola SM, et al. Detecting cognitive
impairment by eye movement analysis using automatic classification
algorithms[ J]. J Neurosci Methods, 2011, 201(1): 196-203.Lagun D, Manzanares C, Zola SM, et al. Detecting cognitive
impairment by eye movement analysis using automatic classification
algorithms[ J]. J Neurosci Methods, 2011, 201(1): 196-203.
71、Pereira ML, Camargo M, Bellan AFR, et al. Visual search efficiency in
mild cognitive impairment and Alzheimer’s disease: an eye movement
study[ J]. J Alzheimers Dis, 2020, 75(1): 261-275.Pereira ML, Camargo M, Bellan AFR, et al. Visual search efficiency in
mild cognitive impairment and Alzheimer’s disease: an eye movement
study[ J]. J Alzheimers Dis, 2020, 75(1): 261-275.