Abstract: Deep anterior lamellar keratoplasty (DALK) is preferred over conventional penetrating keratoplasty (PKP) for the treatment of anterior corneal opacities or ectasias due to decreased risk of endothelial rejection. However, DALK remains surgically challenging, largely due to challenges associated with achieving consistent pneumo-dissection of posterior stroma from the underlying pre-Descemet’s or Descemet’s membrane (DM). Air must be injected at sufficient depth in the corneal stroma in order to achieve successful pneumo-dissection, but advancing a needle too deep into the cornea can lead to perforation of DM. We describe here a novel technique using a handheld slit lamp (Eidolon model 510L, Eidolon Optical LLC, Natick, MA, USA) to assist in creation of the big-bubble in DALK surgery. Use of a handheld slit beam intraoperatively is a safe, relatively inexpensive, and effective technique for increasing the success of big-bubble formation in DALK procedures.
Deep anterior lamellar keratoplasty (DALK) is increasingly seen as a preferred surgical alternative to traditional penetrating keratoplasty (PKP) in patients with isolated corneal stromal scarring or ectasia with normal Descemet’s membrane (DM) and endothelium (1-3). In comparison to PKP, DALK preserves the patient’s own endothelium, thereby essentially eliminating the risk of endothelial immune rejection (4). However, optimal visual acuity is only achieved in DALK when DM is completely bared or only minimal host residual posterior stroma remains (5). In order to bare DM or achieve a clean excision of the majority of the host corneal stroma, multiple techniques have been proposed (1,6). To date, the most popular method for achieving this dissection is the big-bubble technique first described by Anwar et al. in 2002 (7).
The big-bubble technique involves injection of air into the deep posterior stroma of the cornea in order to create a pneumatic dissection plane between pre-Descemet’s layer (type 1 bubble) or DM (type 2 bubble) and the posterior stroma (8). Though effective, this technique is challenging with a steep learning curve (4,9). An adequate injection depth just above DM is required in order to achieve a consistent big-bubble (10). However, under the en face illumination of a surgical scope, the depth of a needle within the thin cornea stroma can often be difficult to assess. Overly aggressive needle placement can result in perforation of DM, which may necessitate conversion to PKP.
Intraoperative ocular coherence tomography (OCT) and femtosecond laser technology have been touted as solutions to this problem, by providing intraoperative confirmation of the depth of needle placement or by providing a pre-cut needle track to the appropriate depth, respectively (10-12). However, the technology is, as of yet, still unrefined. Currently, intraoperative OCT units lack true microscope integrated, real-time surgical scanning capabilities. And femtosecond lasers still lack standardized built-in software protocols for DALK needle-tracks (10-12). Furthermore, the technology remains expensive and most surgeon have limited access to these options.
To that end, we describe here a novel technique for reliably achieving a big-bubble in DALK by using a relatively inexpensive Eidolon model 510L handheld slit lamp (Eidolon Optical LLC, Natick, MA, USA) to guide needle placement.
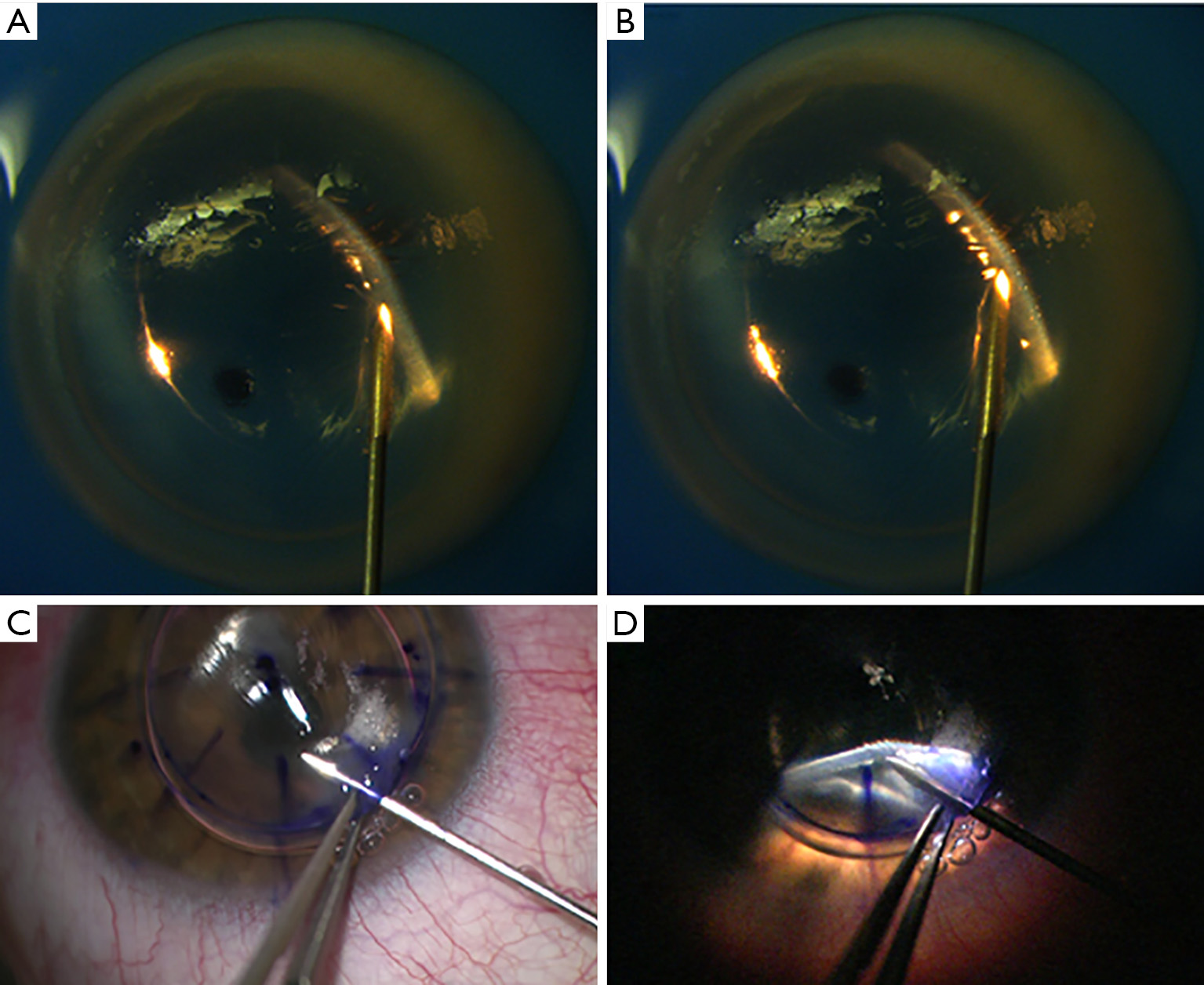
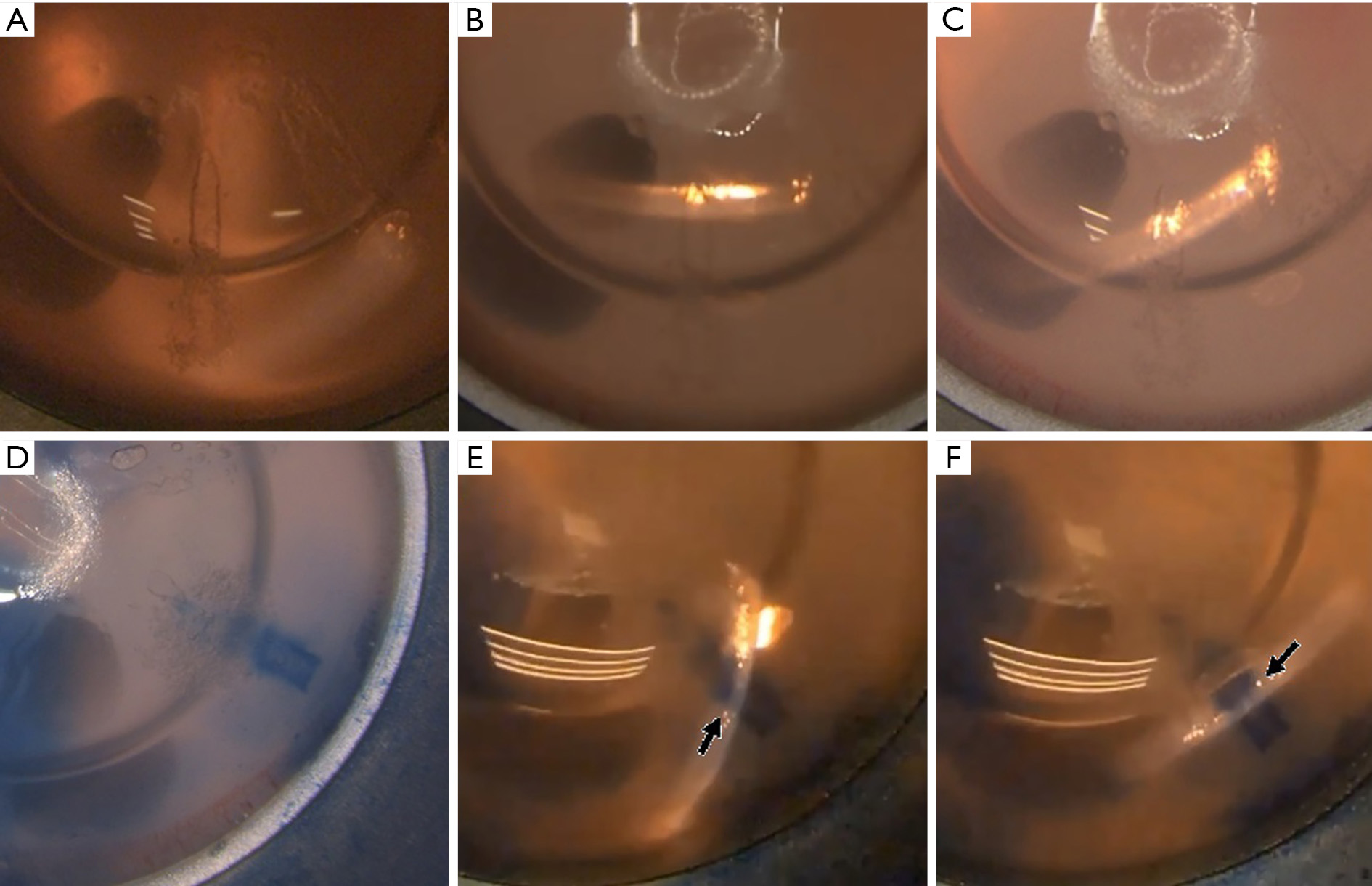
The host cornea is first trephinated to approximately 80% depth. Following trephination, a single paracentesis incision is created. Aqueous is burped from the AC and replacement with a single large air bubble. The use of an air fluid interface to improve visualization of DM was first described by Melles et al. and offers improved visualization even under en face illumination, but is even more effective with slit beam illumination (13). The presence of an air-fluid interface at DM creates bright specular reflection under appropriately positioned slit beam illumination (Figure 1). Care is taken during this step to maintain a low to normal intraocular pressure to ensured lower inflation pressures during big-bubble formation.
Next, using 0.12 forceps for stabilization, a bent 27-gauge needle on a 5 mL syringe is placed into the corneal stroma at the level of the trephination and advanced partially into the host corneal stroma. Alternatively, Fogla or other DALK instruments can be used to begin this initial stromal tunnel. The handheld slit beam is secured into the finger of a sterile surgical glove with a single small area cut at the tip of the finger to allow unimpeded illumination from the device. The slit beam is then positioned over the surgical field by an assistant, with the beam in focus on the cornea (working distance of approximately one inch) and set at its thinnest setting. The slit beam is then oriented 45 degrees to the tip of the needle with the slit beam at the tip or immediately in front of the needle tip to assist with guidance of the needle during advancement to the paracentral deep stroma. Care should be taken to illuminate the cornea obliquely from the periphery to maximize specular reflection. With dimming of the en face illumination of the surgical scope, the slit beam and depth of the needle tip within the cornea stroma is easily appreciated. Gentle sweeps of the slit beam across the needle tip at this point can further highlight the depth of the needle (Figures S1,S2).
DM should also be clearly visible at this point due to the bright reflection off of the air-DM interface. This bright reflection off DM allows clear visualization of a wave like distortion in DM when appropriate depth is achieved (Figure 1). This frequently correlates with a decreased resistance to needle advancement, which has previously been described (14). Once appropriate depth is achieved, air can be injected forcefully until creation of a type 1 big bubble is demonstrated. Alternatively, the needle can be retracted and a DALK cannula can be inserted into the needle track to complete the pneumo-dissection.
If depth of the needle or cannula is difficult to appreciate, a small amount of air or trypan blue can be injected to slightly pneumatize or stain the needle track, respectively (Figure 2). This further enhances the visualization of stromal depth under slit beam illumination.
Following completion of the big bubble and separation of posterior stroma from underlying Pre-Descemet’s membrane, removal of the overlying stroma can be performed as previously described by Anwar and Teichmann (7).
We describe here a novel technique for using a handheld slit lamp to assist in big bubble formation and demonstrate its use both in the lab with cadaveric donor corneas on a false anterior chamber (Figure S1), as well intraoperatively in a patient with keratoconus (Figure S2). Intraoperative use of a portable handheld slit lamp has previously been described in DM endothelial keratoplasty (DMEK) surgery as a reliable method for confirming DMEK graft orientation (15). It has further been described in DALK surgery a means of confirming big-bubble formation (15). However, to the best of our knowledge, use of a handheld slit lamp for real-time guidance of needle placement in order to consistently achieve a big-bubble during DALK surgery has never been described.
By using slit beam illumination, the surgeon is better able to assess his or her needle depth compared to the standard en face illumination of a surgical scope due to direct visualization of the full thickness of the cornea. Use of the slit beam also synergistically improves visualization of DM when combined with placement of a large intracameral air bubble, as described by Melles et al. (13). This, in turn, helps reduce the risk for DM perforation. This synergistic improvement in visualization of DM is achieved because specular reflection from the slit beam illumination off the air-DM interface highlights DM to a degree that is not achievable with standard en face illumination. Though we demonstrate use of the Eidolon slit lamp in DALK surgery using a 27-gauge needle, other DALK instruments or cannulas can just as easily be used with the handheld slit lamp.
DALK surgery remains a challenging procedure for corneal surgeons and creation of a big-bubble remains one of the most difficult steps. Success rates for big-bubble formation range from 65% to 85.3% even in the hands of experienced surgeons (3,16,17). Multiple studies have further acknowledged a steep learning curve with even lower success rates in the hands of inexperienced surgeons (4,9,16). Further studies to evaluate efficacy of this technique in the hands of experienced and inexperienced DALK surgeons will be important moving forward.
A handheld slit lamp has multiple advantages over microscope-mounted slit lamps, including being more flexible in terms of positioning and angling the light beam and being more cost-effective (15). Use of a handheld slit lamp is further advantageous over current intraoperative OCTs since it provides real-time visualization of needle insertion (10,11). Though future advancements in intraoperative OCT and femtosecond laser technology may ultimately lead to more widespread use of those technologies and even higher success rates with big-bubble DALK surgery, use of a handheld slit lamp technique will remain a cost-efficient, simple, and effective alternative.
One limitation to this technique is the need for an assistant to be present to position the slit lamp and intermittently sweep the beam across the needle tip. A possible modification to the technique that could address this issue is potentially using a fixed articulating stand to hold the slit beam in proper position for the unassisted surgeon. Alternatively, even without an assistant the handheld slit beam can still be used to confirm the depth of the needle after it has already been advanced.
In conclusion, the technique described here for use of a handheld slit lamp to assist in big-bubble formation in DALK surgery is an inexpensive and effective method for increasing the success rates for novice surgeons.