Pterygia are an extremely common ocular condition believed to be occurring due to proliferation and overgrowth of abnormal epithelial and fibrovascular tissue onto the cornea.
They are characterized by cellular proliferation, neovascularization and inflammation. Indications for treatment vary from minor cosmetic concerns to significant visual loss. Management options include an array of surgical techniques including simple resection (leaving the sclera bare), or resection followed by covering the sclera with primary conjunctival closure, a conjunctival or conjunctivolimbal autograft (CAG and CLAG respectively) from another site on the bulbar conjunctiva of the same eye, or with human amniotic membrane (HAM). Adjuvants like mitomycin C and 5-fluorouracil have also been used along with the above mentioned surgical techniques in an attempt to reduce recurrence. Also pterygium resection may be combined with or without extensive removal of Tenon’s capsule. The main primary outcome concerns are recurrence of pterygium, cosmesis, other complications like dislocation of conjunctival graft or HAM graft, suture related problems (pain, inflammation, granuloma formation), possible long term complications of mitomycin C whenever used. Secondary outcome concerns are surgically induced refractive changes, duration of surgery, cost of surgery and possible transmission of viral or prion disease because of use of fibrin glue. The reported rate of recurrence shows a wide range (from as low as 2% to as high as 80%), and may be influenced by the surgical technique adopted for pterygium excision (1). Thus one of the major primary aims of a successful pterygium surgery is prevention of recurrences, for which various strategies have evolved over time.
Kenyon et al. (2) in 1985 first described the conjunctival autografting and since then it has become the primary choice for the surgical management (3-6) of this disorder.
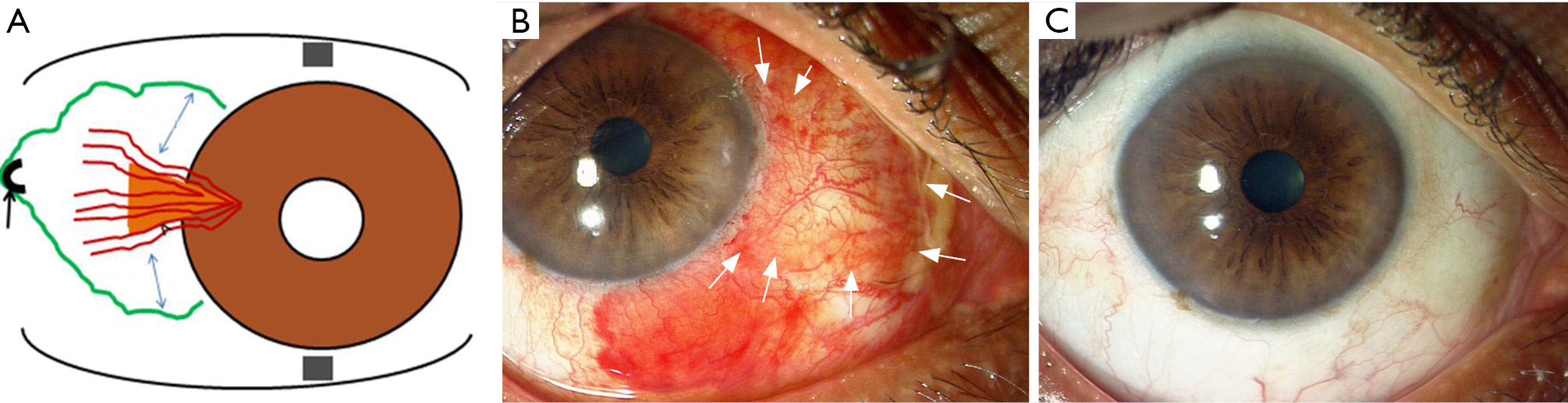
Transplantation of a conjunctival graft with or without inclusion of limbal tissue has been demonstrated to be an effective method to lower the recurrence rates as compared to bare sclera technique. Another strategy to reduce recurrence emphasizes ‘thorough (PERFECT Technique)’ or ‘semi-thorough (CRATER Technique)’ removal of the fibrovascular tissue and Tenon’s layer (Figure 1 and Table 1) (7-10). Recurrences after pterygium excision may be attributable to the production of hyaluronate and scar tissue by stimulated fibroblasts in the Tenon’s capsule and pterygial tissue, as demonstrated by Denk and Kria et al. (11-13) in vitro experimental studies.
| Authors | Study design | Study groups | Sample size | Observations/complications | Recurrence | Follow up |
|---|---|---|---|---|---|---|
| Hirst ( |
Cases series study | PERFECT technique for excision of primary pterygium | 250 consecutive patients | Vascularized dellen in one patient | 0.4% | 462±172 days |
| Hirst ( |
Case series study | Recurrent pterygium excision using PERFECT technique | 111 consecutive patients | Exotropia in one patient; 1 patient lot 4 lines of vision as a result of corneal ulcer | 0% | 1 year |
| Malhotra |
Prospective comparative case series | Fibrin glue assisted CAG |
49 eyes of 47 patients | No significant diplopia in any patient | 0% recurrence in both groups | 63 weeks (range, 54–81 weeks) |
| Bahar |
Retrospective study | Extensive |
135 patients (161 eyes) | Time to recurrence: 4 months in limited excision group |
12.1% in limited excision group |
? |
CAG, conjunctival autograft; CLAG, conjunctivolimbal autograft.
Traditionally the CAG, of late thought to be best method for preventing recurrence of pterygium, is attached to the sclera by suturing. But in last decade the fibrin glue for suture free CAG has been used extensively, as it prevents suture related problems, produces less inflammation and pain, decreases surgical time and possibly may reduce recurrence rates.
Fibrin glue is a two part material consisting of fibrinogen and thrombin, when mixed quickly polymerize to form a complex that is both chemically and ultrastructurally identical to a human plasma clot. Tisseel by Baxter is the most commonly used glue for this purpose. Many studies in the recent past have compared the attachment of the CAG with either fibrin glue or with sutures (14-16) and reported more favorable outcomes with glue in terms of shortening of the surgical time, better patient comfort and reduced recurrence rates.
Zloto et al. (17) from Israel evaluated the surgical outcomes of pterygium excision combined with CAG using either vicryl sutures or fibrin glue from two different manufacturers i.e., Evicel (Omrix Biopharmaceuticals Ltd, Ramat-Gan, Israel) and Tisseel (Baxter Corp., Deerfield, IL, USA). Evicel glue differs from Tisseel glue in that it does not have the bovine protein aprotinin that retards the clot lysis. In this study the authors randomized 89 patients into three groups and followed them up for 3 months. They have also compared the two commonly used fibrin glues which have not been studied earlier. Their results showed that the pterygium recurrence, patient discomfort level and surgery time were reduced markedly in the fibrin group as compared to sutures group which was quite consistent with the earlier published studies (14-16). They found Tisseel glue, in addition to be more cost effective than Evicel and vicryl sutures, to be better than the Evicel glue in terms of complications such as flap dislocation and pterygium recurrence. Evicel group had five cases of graft dislocation as compared to none in Tisseel group. Authors believe that those differences were caused by the differences in adhesive strength between the glues. Aprotinin and factor 13 are components of Tisseel fibrin glue, but not of Evicel fibrin glue. Aprotinin is a synthetic component used as a polyvalent protease inhibitor that prevents premature degradation of fibrin. Factor 13, which also exists in the human coagulation cascade, is a fibrin-stabilizing factor that cross-links the fibrin. Authors believe that those components strengthen the fibrin clot created by Tisseel and make it stronger than the fibrin clot created by Evicel.
The meta-analysis by Pan et al. (18) of randomized control trials evaluating CAG to cover the bare sclera left behind after pterygium excision supports the superiority of fibrin glue over sutures in significantly reducing the recurrence rate without an apparent increased risk of complications. Romano et al. (19) in Cochrane database of systematic reviews, 2016 which has included 14 studies, concluded that for every 100 cases operated, the use of fibrin glue would be associated with approximately five lesser recurrences as compared to sutures. Analysis of 9 RCTs in this meta-analysis which reported on surgical duration, showed that surgical times using glue were shorter by approximately 17 minutes when compared with using sutures. However in contrast to the meta-analysis by Pan et al. (18) the complication rate (e.g., dehiscence or retraction of the graft, formation of granuloma) in the meta-analysis conducted by Romano et al. (19) was higher with the use of fibrin glue as compared to sutures. Though their results reported a higher complication rate in fibrin glue group but it was seen that complication rates mainly depend on graft preparation, graft manipulation, surgical experience, and participant selection. Conjunctival graft preparation has to be meticulous in the sense that it should be properly sized, as thin as possible without button holes and preferably with no or minimal amount of Tenon’s capsular fascia. Graft dehiscence which is the most common complication in the fibrin group is usually associated with eye trauma or a person rubbing their eyes (20).
One of the concerns with use of fibrin glue is the possibility of transmitting infectious agents. So far there is no report yet documenting the transmission of infectious agent with the use of fibrin glue, but the risk cannot be completely ruled out. To circumvent this problem, Bondalapati and Ambati (21) in 9 eyes of 7 patients undergoing pterygium excision, utilized ReSure? tissue sealant (Ocular Therapeutix, Bedford, MA, USA), for fixing an HAM transplant to the bare sclera. ReSure? was originally approved by the FDA for sealing corneal incisions after cataract surgery. It consists of two separate components: a polyethylene glycol solution and a trilysine amine solution, which when combined acquire sealant properties. In contrast to fibrin glue, ReSure? does not carry the risk of viral transmission. The tissue sealant was applied at the edges of the donor amniotic membrane and host conjunctiva surrounding the bare sclera bed. The authors did not report any case of dislocation of the amniotic membrane or recurrence of the pterygium in the follow up period. They also noted ease of application and reduced patient discomfort in the post operative period. In contrast, Hirst (22) using ReSure? to adhere the CAG after excision of the pterygium, noted less favourable outcomes of conjunctival scarring preceded by a prolonged inflammatory phase. According to Bondalapati and Ambati (21) this could be due to a direct application of ReSure?, to the surgical bed instead of application at the edges.
In another Cochrane Systematic Review (23) which included 20 randomized controlled trials, the authors compared the effects of CAG relative to HAM transplant with respect to pterygium recurrence at 3 and 6 months after surgery and found no statistically significant difference in risk of recurrence for primary or recurrent pterygia 3 months after surgery; at 6 months, among 1,021 eyes in 10 RCTs, CAG conferred a 47% lower risk of recurrence than did the HAM transplant. Although at 6 months after surgery subgroup analysis showed no difference in recurrence between the two procedures performed for primary pterygia, for the 96 eyes with recurrent pterygia at baseline, CAG transplantation was associated with a 55% lower risk of recurrence compared to the HAM transplantation. Authors concluded CAG was more effective than amniotic membrane transplantation to prevent pterygium recurrence by 6 months post surgery, especially in recurrent pterygia. We also reported a zero recurrence rate using fibrin glue in primary pterygium surgery utilizing HAM, which was transplanted with a novel ‘tuck-in’ technique (24).
The debate on the best modality for pterygium surgery, i.e., fixation of the conjunctival graft with fibrin glue or sutures has been continuing for the last decade, with both approaches having their strengths and weaknesses in terms of duration of the surgical procedure, intra and post operative complications, patient comfort and recurrence rates. Kurian et al. (25) described utilization of autologous blood for fixing the CAG. In their randomized controlled trial evaluating autologous blood with fibrin glue for graft fixation. The graft dislodgement and recurrence rates were 3.13% and 6.25% respectively for the former group and 2.04% and 8.16% respectively for the latter.
According to the authors, the comparable long term outcomes and complication rates, represented a promising potential for autologous blood to be used as a substitute for fibrin glue, simultaneously also reducing the dreaded complications of transmission of viral disease and anaphylactic reaction to fibrin glue.
In conclusion, future randomized controlled trials or Cochrane database of systematic reviews should focus on addressing changes in patient-reported outcomes (symptoms, cosmesis) and visual acuity, and evaluate effects of surgical variations like use of adjunctive mitomycin C or extended removal of Tenon’s capsule.