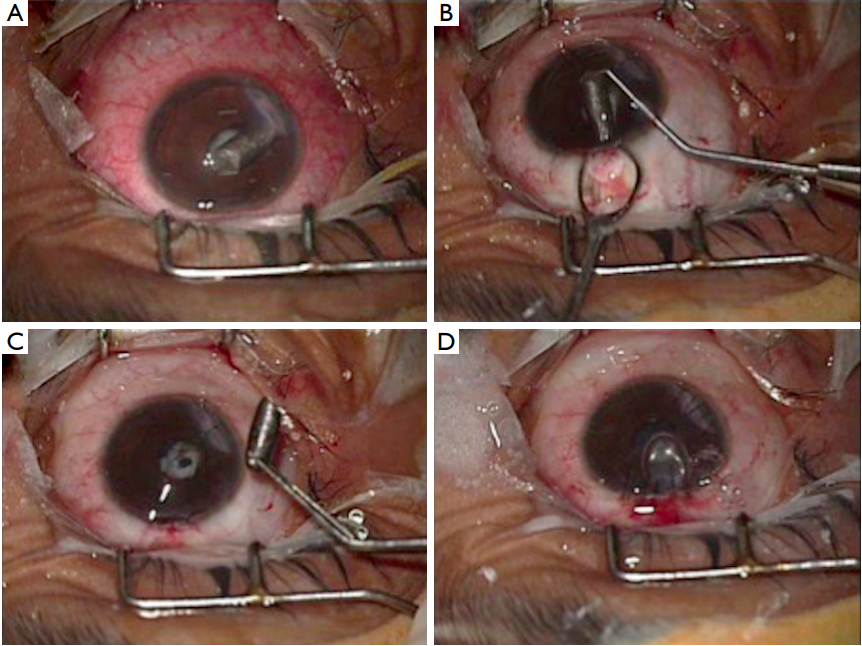
We report a case of large graphite foreign body (FB) in the anterior chamber of eye of a 4-yearold
child, incurred during unsupervised play. Despite delayed presentation, the eye had few signs of resolved
inff ammation which allowed safe extraction of the FB bimanually through limbus. School play, especially in
young children, should be under supervision and free of sharp objects. Graphite is inert while inside the eye,
and even large pieces can be well tolerated for long time in absence of infection.