
患者,女性,73岁,因“右眼外伤后视力下降30年,突发眼红痛4 d”于2017年5月23日入院。患者30余年前因农作时被木柴打伤右眼,视力明显下降,当时未诊治。4 d前突发右眼眼红、眼痛,遂到当地医院就诊,予妥布霉素地塞米松滴眼液、噻吗心安滴眼液及甘露醇治疗,症状无缓解转来广东省人民医院。患者否认既往糖尿病、高血压病、冠心病病史。眼部体查:右眼视力,光感/定位准,红绿可辨;左眼视力0.1,矫正至0.4。右眼眼压28 mmHg(1 mmHg=0.133 kPa),左眼眼压17 mmHg。右眼结膜充血,鼻侧纤维血管膜长入角膜约2 mm,尖端指向瞳孔,角膜雾状水肿,前房无晶状体深,Tyn(+),虹膜震颤,纹理窥不清,瞳孔4 mm×4 mm,对光反射(−),晶状体缺如,眼底窥不清。左眼角膜透明,前房中深,瞳孔3 mm×3 mm,对光反射存在,晶状体浑浊C2N3P1,眼底除后极部散在玻璃膜疣外,未见明显异常。辅助检查:眼部B超示右眼玻璃体混浊,晶状体完全脱位于视乳头上方(图1)。光学相干断层扫描(optical coherence tomography,OCT)示左眼黄斑区未见明显异常。诊断:1 )右眼继发性青光眼;2)右眼晶状体完全脱位;3)右眼翼状胬肉;4 )左眼老年性白内障;5 )左眼屈光不正。患者入院予全身及局部激素抗炎、局部降眼压(布林佐胺滴眼液、酒石酸溴莫尼定滴眼液、噻吗心安滴眼液)、保护角膜、预防感染等治疗。入院第3天时在球后睫状神经阻滞麻醉下行右眼玻璃体切除+晶状体咬切术。手术当天术前右眼眼压28 mmHg,视力为手动/眼前,角膜水肿较前缓解,余眼部体查大致同前。术中见玻璃体絮状混浊,晶状体完全脱位于视乳头上方。切除混浊玻璃体,玻切头咬切晶状体皮质,见棕黄色晶状体核,置晶状体核于前房,做上方角膜缘切口挽出晶状体核。挽核瞬间患者出现烦躁不安,诉眼部胀痛,手术显微镜下见瞳孔区红光反射消失,前房变浅,上方虹膜从角膜缘切口脱出、玻璃体溢出,眼底见鼻侧及颞侧脉络膜棕红色球形隆起,对吻面积大,窥不清眼底视乳头及黄斑区结构(图2)。考虑SEH,立刻关闭角膜缘切口。术后予止血、止痛、镇静、脱水等治疗,患者诉眼痛较术中略减轻,可忍受。术后第1天,患者右眼视力手动/20 cm,眼压7.5 mmHg,右眼角膜轻度水肿,后弹力层皱褶,房水轻混,上方虹膜嵌顿于角膜缘切口,前房深,瞳孔向上移位(图3A),前置镜下隐约见眼底颞侧脉络膜隆起,余结构窥不清。眼部B超示:右眼脉络膜上腔出血(图3B)。当日在表面麻醉下行右眼虹膜还纳术。术后第2天,右眼视力手动/20 cm,眼压7.5 mmHg,右眼虹膜已还纳,瞳孔近圆形,余体查大致同前。术后第6天,右眼视力指数/眼前(颞侧),眼压15.2 mmHg,角膜水肿基本消退,角膜后弹力层皱褶消退,眼前段体查大致同前(图4A),眼底见颞侧和鼻侧脉络膜视网膜球形隆起,隐约见视盘(图4B)。B超示:右眼脉络膜脱离范围较前减小,脉络膜上腔出血较前吸收(图4C)。患者病情基本稳定,诉无特殊不适,予带药出院。术后第13天复诊,右眼视力指数/眼前(颞侧),眼压10.9 mmHg,角膜透明,房水清,玻璃体前散在虹膜色素附着(图5A),眼底见颞侧和鼻侧脉络膜视网膜球形隆起,视盘可见(图5B),余体查大致同前。术后第27天复诊,右眼视力0.01,+12.00 DS/−6.00 DC ×40°矫至0.15+2,眼压8.2 mmHg,右眼角膜透明,房水清,前房深,瞳孔水滴样颞上移位,对光反射迟钝(图6A),眼底后极部显露,隐约见豹纹状视网膜改变(图6B)。眼部B超示:右眼脉络膜脱离范围较前明显减小(图6C)。
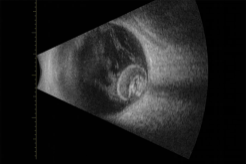
图1 术前眼部B超示右眼玻璃体混浊,晶状体完全脱位于 视乳头上方
Figure 1 Preoperative ocular B ultrasound showed the vitreous opacity and lens completely dislocated above the optic nerve in the right eye
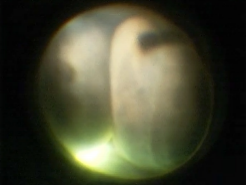
图2 术中显微镜下见鼻侧及颞侧视网膜脉络膜棕红色球形 隆起,对吻面积大,窥不清眼底视乳头及黄斑区结构
Figure 2 Under the microscope, two brown-red spherical chorioretinal bulges from the nasal and temporal sides with a large area covered the optic disc and themaculararea

图3 术后第1天
Figure 3 The first day after surgery
(A)右眼角膜轻度水肿,后弹力层皱褶,上方虹膜嵌顿于角膜缘切口,瞳孔向上移位; (B)B超示右眼脉络膜上腔出血。
(A)The corneal of the right eye was mild edema with the folds of the corneal posterior elastic layer, part of the iris incarcerated in the corneal incision, and the pupil shifted upward; (B) Ocular B ultrasound showed the suprachoroidal hemorrhage in the right eye.
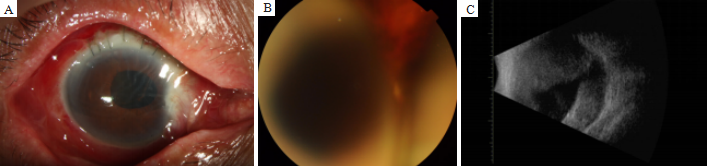
图4 术后第6天
Figure 4 The 6th day after surgery
(A)右眼虹膜还纳,瞳孔近圆形; (B)眼底见颞侧和鼻侧脉络膜视网膜球形隆起,隐约见视盘; (C) B超示右眼脉络膜脱离范 围较前减小,脉络膜上腔出血较前吸收。
(A)The iris of the right eye returned to the anterior chamber and the pupil was nearly round; (B) Two brown-red spherical chorioretinal bulges were shown in the fundus with the optic disc visible vaguely; (C) Ocular B ultrasound showed the reducing of choroidal detachment as well as the absorption of the suprachoroidal hemorrhage in the right eye.
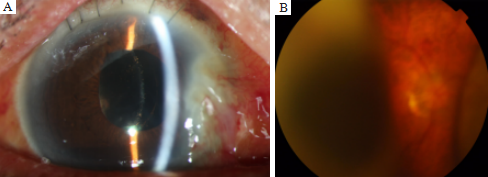
图5 术后第13天
Figure 5 The 13th day after surgery
(A)右眼角膜透明,房水清,玻璃体前散在虹膜色素附着; (B)眼底见颞侧和鼻侧脉络膜视网膜球形隆起变小,视盘可见。
(A)The corneal and aqueous humor was clear, and iris pigment diffused in front of the vitreous; (B) The temporal and nasal chorioretinal bulges were smaller and the optic disc was visible in the right eye.
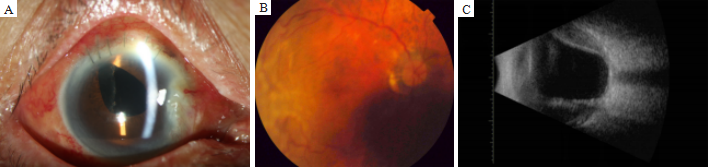
图6 术后第27天
Figure 6 The 27th day after surgery
(A)右眼角膜透明,房水清,前房深,瞳孔水滴样颞上移位; (B)眼底见脉络膜脱离较前明显减轻,可见视盘及黄斑区;(C)B超示右眼脉络膜脱离范围较前明显减小。
(A)The corneal and aqueous humor was clear, the anterior chamber was deep, and the pupil shifted to the temporal and upper side, like a water drop; (B) The choroidal detachment obviously reduced, with the optic disc and macular area visible; (C) Ocular B ultrasound showed the choroidal detachment obviously reduced in the right eye.
脉络膜上腔出血又称驱逐性出血,是内眼手术中(暴发性)或术后(迟发性)出现的严重并发症,临床上较少见但破坏性极为严重[1]。其发病机制多认为由眼内压过低,睫状后长或后短动脉破裂或大血管支的动静脉部分破裂所致[2-3]。其诱发因素多种,全身危险因素包括:高龄、高血压、糖尿病、动脉粥样硬化、凝血功能障碍等[4]。眼部危险因素包括:青光眼、白内障、眼内炎症、高度近视及既往内眼手术史等[5]。术中或术后眼压急骤降低和持续的低眼压被认为是驱逐性脉络膜上腔出血的诱因之一。同时,患者紧张、术中屏气、咳嗽等亦可诱发脉络膜上腔出血。本例患者73岁高龄,出现继发性青光眼、核性晶状体、挽出晶体核瞬间眼压骤降,都是引起脉络膜上腔出血的原因。术中一旦出现SEH,治疗关键为及时发现,迅速关闭切口,控制眼压,全身及局部使用皮质类固醇激素减轻眼部炎症,止痛剂、止血剂、镇静剂等酌情使用[6]。术后应定期复查眼部B超,了解眼底出血吸收情况,必要时可在术后2周左右行巩膜切开脉络膜上腔放液及玻璃体视网膜手术。为避免SEH,应根据每位患者全身及眼部情况制定个体化治疗方案,排除全身高危因素,术前控制眼压,做好宣教,安抚患者紧张情绪,避免术中屏气、咳嗽等举止;术中注意手术切口不宜过大,避免眼压巨幅波动,动作轻巧,手术时间尽量缩短。及时且正确的处理,可最大程度的挽救患者视力,提高其生活质量。


点击右上角菜单,浏览器打开下载