1、Latif F, Tory K, Gnarra J, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993, 260(5112): 1317-1320. DOI: 10.1126/science.8493574.Latif F, Tory K, Gnarra J, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993, 260(5112): 1317-1320. DOI: 10.1126/science.8493574.
2、Nordstrom-O’Brien M, van der Luijt RB, van Rooijen E, et al. Genetic analysis of von Hippel-Lindau disease. HumMutat. 2010, 31(5): 521-537. DOI: 10.1002/humu.21219.Nordstrom-O’Brien M, van der Luijt RB, van Rooijen E, et al. Genetic analysis of von Hippel-Lindau disease. HumMutat. 2010, 31(5): 521-537. DOI: 10.1002/humu.21219.
3、Louise M Binderup M, Smerdel M, Borgwadt L, et al. von Hippel-Lindau disease: Updated guideline for diagnosis and surveillance. Eur J Med Genet.2022, 65(8):104538.
DOI: 10.1016/j.ejmg.2022.104538.Louise M Binderup M, Smerdel M, Borgwadt L, et al. von Hippel-Lindau disease: Updated guideline for diagnosis and surveillance. Eur J Med Genet.2022, 65(8):104538.
DOI: 10.1016/j.ejmg.2022.104538.
4、Varshney N, Kebede AA, Owusu-Dapaah H, et al. A review of von hippel-lindau syndrome. J Kidney Cancer VHL. 2017, 4(3): 20-29. DOI: 10.15586/jkcvhl.2017.88.Varshney N, Kebede AA, Owusu-Dapaah H, et al. A review of von hippel-lindau syndrome. J Kidney Cancer VHL. 2017, 4(3): 20-29. DOI: 10.15586/jkcvhl.2017.88.
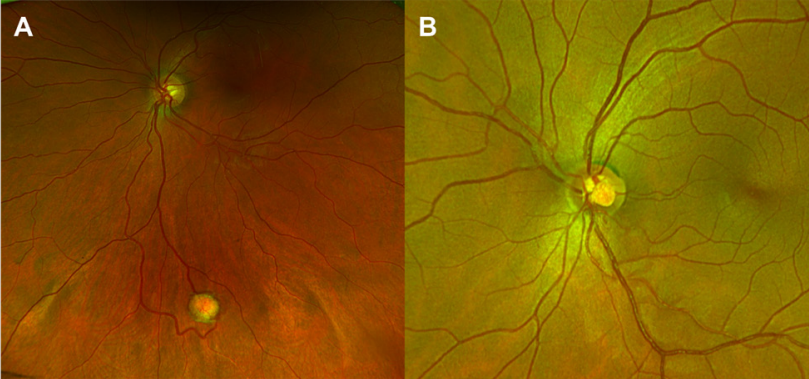
5、Welch RB. Von Hippel-Lindau disease: the recognition and treatment of early angiomatosis retinae and the use of cryosurgery as an adjunct to therapy. Trans Am
Ophthalmol Soc. 1970, 68: 367-424.Welch RB. Von Hippel-Lindau disease: the recognition and treatment of early angiomatosis retinae and the use of cryosurgery as an adjunct to therapy. Trans Am
Ophthalmol Soc. 1970, 68: 367-424.
6、Webster AR, Maher ER, Moore AT. Clinical characteristics of ocular angiomatosis in von Hippel-Lindau disease and correlation with germline mutation. Arch Ophthalmol.
1999, 117(3): 371-378. DOI: 10.1001/archopht.117.3.371.Webster AR, Maher ER, Moore AT. Clinical characteristics of ocular angiomatosis in von Hippel-Lindau disease and correlation with germline mutation. Arch Ophthalmol.
1999, 117(3): 371-378. DOI: 10.1001/archopht.117.3.371.
7、Dollfus H, Massin P, Taupin P, et al. Retinal hemangioblastoma in von Hippel-Lindau disease: a clinical and molecular study. Invest Ophthalmol Vis Sci.
2002, 43(9): 3067-3074.Dollfus H, Massin P, Taupin P, et al. Retinal hemangioblastoma in von Hippel-Lindau disease: a clinical and molecular study. Invest Ophthalmol Vis Sci.
2002, 43(9): 3067-3074.
8、Chew EY. Ocular manifestations of von Hippel-Lindau disease: clinical and genetic investigations. Trans Am Ophthalmol Soc. 2005, 103: 495-511.Chew EY. Ocular manifestations of von Hippel-Lindau disease: clinical and genetic investigations. Trans Am Ophthalmol Soc. 2005, 103: 495-511.
9、McCabe CM, Flynn HW Jr, Shields CL, et al. Juxtapapillary capillary hemangiomas. Clinical features and visual acuity outcomes. Ophthalmology. 2000,
107(12): 2240-2248. DOI: 10.1016/s0161-6420(00)00422-x.McCabe CM, Flynn HW Jr, Shields CL, et al. Juxtapapillary capillary hemangiomas. Clinical features and visual acuity outcomes. Ophthalmology. 2000,
107(12): 2240-2248. DOI: 10.1016/s0161-6420(00)00422-x.
10、Chan CC, Vortmeyer AO, Chew EY, et al. VHL gene deletion and enhanced VEGF gene expression detected in the stromal cells of retinal angioma. Arch Ophthalmol.
1999, 117(5): 625-630. DOI: 10.1001/archopht.117.5.625.Chan CC, Vortmeyer AO, Chew EY, et al. VHL gene deletion and enhanced VEGF gene expression detected in the stromal cells of retinal angioma. Arch Ophthalmol.
1999, 117(5): 625-630. DOI: 10.1001/archopht.117.5.625.
11、Nicholson DH, Green WR, Kenyon KR. Light and electron microscopic study of early lesions in angiomatosis retinae. Am J Ophthalmol. 1976, 82(2): 193-204. DOI:
10.1016/0002-9394(76)90418-9.Nicholson DH, Green WR, Kenyon KR. Light and electron microscopic study of early lesions in angiomatosis retinae. Am J Ophthalmol. 1976, 82(2): 193-204. DOI:
10.1016/0002-9394(76)90418-9.
12、Chan CC, Lee YS, Zhuang Z, et al. Von Hippel-Lindau gene deletion and expression of hypoxia-inducible factor and ubiquitin in optic nerve hemangioma.
TransAmOphthalmolSoc. 2004, 102: 75-79;discussion 79-81.Chan CC, Lee YS, Zhuang Z, et al. Von Hippel-Lindau gene deletion and expression of hypoxia-inducible factor and ubiquitin in optic nerve hemangioma.
TransAmOphthalmolSoc. 2004, 102: 75-79;discussion 79-81.
13、Jr KAG. Mutation and cancer: statistical study of retinoblastoma. ProcNatlAcadSciUSA. 1971, 68(4): 820-823. DOI: 10.1073/pnas.68.4.820.Jr KAG. Mutation and cancer: statistical study of retinoblastoma. ProcNatlAcadSciUSA. 1971, 68(4): 820-823. DOI: 10.1073/pnas.68.4.820.
14、Knudson AG Jr, Strong LC. Mutation and cancer: neuroblastoma and pheochromocytoma. Am J Hum Genet. 1972, 24(5): 514-532.Knudson AG Jr, Strong LC. Mutation and cancer: neuroblastoma and pheochromocytoma. Am J Hum Genet. 1972, 24(5): 514-532.
15、Knudson A. Genetics of human cancer. Annu Rev Genet. 1986, 20: 231-251. DOI: 10.1146/annurev.genet.20.1.231.Knudson A. Genetics of human cancer. Annu Rev Genet. 1986, 20: 231-251. DOI: 10.1146/annurev.genet.20.1.231.
16、Murgia A, Martella M, Vinanzi C, et al. Somatic mosaicism in von hippel-lindau disease. Hum Mutat. 2000, 15(1): 114. DOI: 10.1002/(SICI)1098-1004(200001)15:
1<114: AID-HUMU20>3.0.CO;2-7.Murgia A, Martella M, Vinanzi C, et al. Somatic mosaicism in von hippel-lindau disease. Hum Mutat. 2000, 15(1): 114. DOI: 10.1002/(SICI)1098-1004(200001)15:
1<114: AID-HUMU20>3.0.CO;2-7.
17、Prowse AH, Webster AR, Richards FM, et al. Somatic inactivation of the VHL gene in Von Hippel-Lindau disease tumors. Am J Hum Genet. 1997, 60(4): 765-771.Prowse AH, Webster AR, Richards FM, et al. Somatic inactivation of the VHL gene in Von Hippel-Lindau disease tumors. Am J Hum Genet. 1997, 60(4): 765-771.
18、Shanbhogue KP, Hoch M, Fatterpaker G, etal. Von hippel�lindau disease: review of genetics and imaging. Radiol Clin North Am. 2016, 54(3): 409-422. DOI: 10.1016/j.rcl.2015.12.004.Shanbhogue KP, Hoch M, Fatterpaker G, etal. Von hippel�lindau disease: review of genetics and imaging. Radiol Clin North Am. 2016, 54(3): 409-422. DOI: 10.1016/j.rcl.2015.12.004.
19、Conway J E , Chou D , Clatter buck R E , etal . Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease.Neurosurgery. 2001, 48(1): 55-62; discussion 62-63. DOI: 10.1097/00006123-200101000-00009.Conway J E , Chou D , Clatter buck R E , etal . Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease.Neurosurgery. 2001, 48(1): 55-62; discussion 62-63. DOI: 10.1097/00006123-200101000-00009.
20、Jr KWG. The von Hippel-Lindau gene, kidney cancer, and oxygen sensing. J Am Soc Nephrol. 2003, 14(11): 2703-2711. DOI: 10.1097/01.asn.0000092803.69761.41.Jr KWG. The von Hippel-Lindau gene, kidney cancer, and oxygen sensing. J Am Soc Nephrol. 2003, 14(11): 2703-2711. DOI: 10.1097/01.asn.0000092803.69761.41.
21、Gossage L, Eisen T, Maher ER. VHL, the story of a tumour suppressor gene. Nat Rev Cancer. 2015, 15(1): 55-64. DOI: 10.1038/nrc3844.Gossage L, Eisen T, Maher ER. VHL, the story of a tumour suppressor gene. Nat Rev Cancer. 2015, 15(1): 55-64. DOI: 10.1038/nrc3844.
22、Nielsen SM, Rhodes L, Blanco I, et al. Von hippel-lindau disease: genetics and role of genetic counseling in a multiple neoplasia syndrome. J Clin Oncol. 2016, 34(18):
2172-2181. DOI: 10.1200/JCO.2015.65.6140.Nielsen SM, Rhodes L, Blanco I, et al. Von hippel-lindau disease: genetics and role of genetic counseling in a multiple neoplasia syndrome. J Clin Oncol. 2016, 34(18):
2172-2181. DOI: 10.1200/JCO.2015.65.6140.
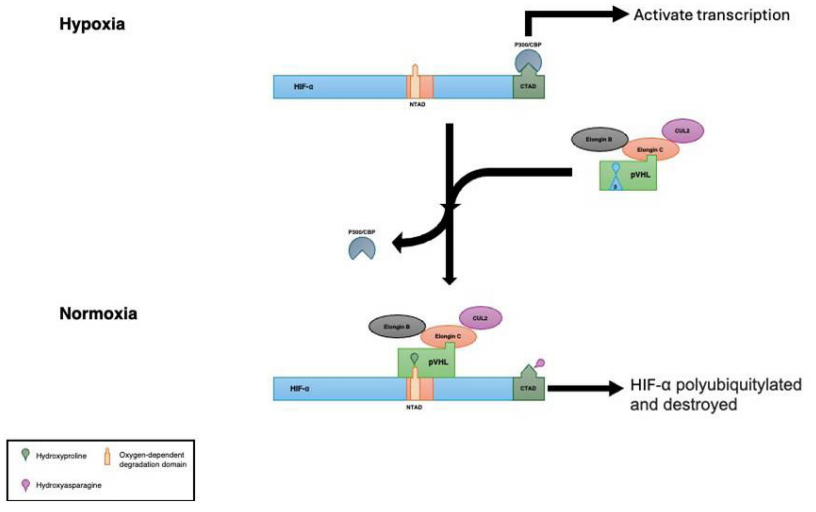
23、Duan DR, Pause A, Burgess WH, et al. Inhibition of transcription elongation by the VHL tumor suppressor protein. Science. 1995, 269(5229): 1402-1406. DOI:
10.1126/science.7660122.Duan DR, Pause A, Burgess WH, et al. Inhibition of transcription elongation by the VHL tumor suppressor protein. Science. 1995, 269(5229): 1402-1406. DOI:
10.1126/science.7660122.
24、Kibel A, Iliopoulos O, DeCaprio JA, et al. Binding of the von Hippel-Lindau tumor suppressor protein to Elongin B and C. Science. 1995, 269(5229): 1444-1446. DOI:
10.1126/science.7660130.Kibel A, Iliopoulos O, DeCaprio JA, et al. Binding of the von Hippel-Lindau tumor suppressor protein to Elongin B and C. Science. 1995, 269(5229): 1444-1446. DOI:
10.1126/science.7660130.
25、Pause A, Lee S, Worrell RA, et al. The von Hippel-Lindau tumor-suppressor gene product forms a stable complex with human CUL-2, a member of the Cdc53 family of
proteins. Proc Natl Acad Sci USA. 1997, 94(6): 2156-2161. DOI: 10.1073/pnas.94.6.2156.Pause A, Lee S, Worrell RA, et al. The von Hippel-Lindau tumor-suppressor gene product forms a stable complex with human CUL-2, a member of the Cdc53 family of
proteins. Proc Natl Acad Sci USA. 1997, 94(6): 2156-2161. DOI: 10.1073/pnas.94.6.2156.
26、Staller P, Sulitkova J, Lisztwan J, et al. Chemokine receptor CXCR4 downregulated by von Hippel-Lindau tumour suppressor pVHL. Nature. 2003, 425(6955): 307-
311. DOI: 10.1038/nature01874.Staller P, Sulitkova J, Lisztwan J, et al. Chemokine receptor CXCR4 downregulated by von Hippel-Lindau tumour suppressor pVHL. Nature. 2003, 425(6955): 307-
311. DOI: 10.1038/nature01874.
27、Rosner I, Bratslavsky G, Pinto PA, et al. The clinical implications of the genetics of renal cell carcinoma. Urol Oncol.2009,27(2):131-136.DOI: 10.1016/j.urolonc.2008.11.001.Rosner I, Bratslavsky G, Pinto PA, et al. The clinical implications of the genetics of renal cell carcinoma. Urol Oncol.2009,27(2):131-136.DOI: 10.1016/j.urolonc.2008.11.001.
28、Singer EA, Bratslavsky G, Middelton L, et al. Impact of genetics on the diagnosis and treatment of renal cancer. Curr Urol Rep. 2011, 12(1): 47-55. DOI: 10.1007/s11934-010-0156-y.Singer EA, Bratslavsky G, Middelton L, et al. Impact of genetics on the diagnosis and treatment of renal cancer. Curr Urol Rep. 2011, 12(1): 47-55. DOI: 10.1007/s11934-010-0156-y.
29、Gradin K, McGuire J, Wenger RH, et al. Functional interference between hypoxia and dioxin signal transduction pathways: competition for recruitment of the Arnt transcription factor. Mol Cell Biol. 1996, 16(10): 5221-5231. DOI: 10.1128/MCB.16.10.5221.Gradin K, McGuire J, Wenger RH, et al. Functional interference between hypoxia and dioxin signal transduction pathways: competition for recruitment of the Arnt transcription factor. Mol Cell Biol. 1996, 16(10): 5221-5231. DOI: 10.1128/MCB.16.10.5221.
30、Huang LE, Arany Z, Livingston DM, et al. Activation of hypoxia-inducible transcription factor depends primarily upon redox-sensitive stabilization of its alpha subunit. J
Biol Chem. 1996, 271(50): 32253-32259. DOI: 10.1074/jbc.271.50.32253Huang LE, Arany Z, Livingston DM, et al. Activation of hypoxia-inducible transcription factor depends primarily upon redox-sensitive stabilization of its alpha subunit. J
Biol Chem. 1996, 271(50): 32253-32259. DOI: 10.1074/jbc.271.50.32253
31、Salceda S, Caro J. Hypoxia-inducible factor 1alpha (HIF-1alpha) protein is rapidly degraded by the ubiquitin�proteasome system under normoxic conditions.Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem. 1997, 272(36): 22642-22647. DOI: 10.1074/jbc.272.36.22642.Salceda S, Caro J. Hypoxia-inducible factor 1alpha (HIF-1alpha) protein is rapidly degraded by the ubiquitin�proteasome system under normoxic conditions.Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem. 1997, 272(36): 22642-22647. DOI: 10.1074/jbc.272.36.22642.
32、Huang LE, Gu J, Schau M, et al. Regulation of hypoxia�inducible factor 1alpha is mediated by an O2-dependent degradation domain via the ubiquitin-proteasome pathway. ProcNatlAcadSciUSA. 1998, 95(14): 7987-7992. DOI: 10.1073/pnas.95.14.7987.Huang LE, Gu J, Schau M, et al. Regulation of hypoxia�inducible factor 1alpha is mediated by an O2-dependent degradation domain via the ubiquitin-proteasome pathway. ProcNatlAcadSciUSA. 1998, 95(14): 7987-7992. DOI: 10.1073/pnas.95.14.7987.
33、Iliopoulos O, Kibel A, Gray S, et al. Tumour suppression by the human von Hippel-Lindau gene product. Nat Med. 1995, 1(8): 822-826. DOI: 10.1038/nm0895-822.Iliopoulos O, Kibel A, Gray S, et al. Tumour suppression by the human von Hippel-Lindau gene product. Nat Med. 1995, 1(8): 822-826. DOI: 10.1038/nm0895-822.
34、Iliopoulos O, Levy AP, Jiang C, et al. Negative regulation of hypoxia-inducible genes by the von Hippel-Lindau protein. Proc Natl Acad Sci USA. 1996, 93(20): 10595-10599. DOI: 10.1073/pnas.93.20.10595.Iliopoulos O, Levy AP, Jiang C, et al. Negative regulation of hypoxia-inducible genes by the von Hippel-Lindau protein. Proc Natl Acad Sci USA. 1996, 93(20): 10595-10599. DOI: 10.1073/pnas.93.20.10595.
35、Kaelin WG Jr, Maher ER. The VHL tumour-suppressor gene paradigm. Trends Genet. 1998, 14(10): 423-426. DOI: 10.1016/s0168-9525(98)01558-3.Kaelin WG Jr, Maher ER. The VHL tumour-suppressor gene paradigm. Trends Genet. 1998, 14(10): 423-426. DOI: 10.1016/s0168-9525(98)01558-3.
36、Maxwell PH, Wiesener MS, Chang GW, et al. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature. 1999,
399(6733): 271-275. DOI: 10.1038/20459.Maxwell PH, Wiesener MS, Chang GW, et al. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature. 1999,
399(6733): 271-275. DOI: 10.1038/20459.
37、Ohh M, Park CW, Ivan M, et al. Ubiquitination of hypoxia�inducible factor requires direct binding to the beta-domain of the von Hippel-Lindau protein. Nat Cell Biol. 2000,
2(7): 423-427. DOI: 10.1038/35017054.Ohh M, Park CW, Ivan M, et al. Ubiquitination of hypoxia�inducible factor requires direct binding to the beta-domain of the von Hippel-Lindau protein. Nat Cell Biol. 2000,
2(7): 423-427. DOI: 10.1038/35017054.
38、Tanimoto K, Makino Y, Pereira T, et al. Mechanism of regulation of the hypoxia-inducible factor-1 alpha by the von Hippel-Lindau tumor suppressor protein.
EMBO J. 2000, 19(16): 4298-4309. DOI: 10.1093/emboj/19.16.4298.Tanimoto K, Makino Y, Pereira T, et al. Mechanism of regulation of the hypoxia-inducible factor-1 alpha by the von Hippel-Lindau tumor suppressor protein.
EMBO J. 2000, 19(16): 4298-4309. DOI: 10.1093/emboj/19.16.4298.
39、Jaakkola P, Mole DR, Tian YM, et al. Targeting of HIF�alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001,
292(5516): 468-472. DOI: 10.1126/science.1059796.Jaakkola P, Mole DR, Tian YM, et al. Targeting of HIF�alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001,
292(5516): 468-472. DOI: 10.1126/science.1059796.
40、Ivan M, Kondo K, Yang H, et al. HIF alpha targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science. 2001, 292(5516):
464-468. DOI: 10.1126/science.1059817.Ivan M, Kondo K, Yang H, et al. HIF alpha targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science. 2001, 292(5516):
464-468. DOI: 10.1126/science.1059817.
41、Hon WC, Wilson MI, Harlos K, et al. Structural basis for the recognition of hydroxyproline in HIF-1α by pVHL. Nature. 2002, 417: 975-978. DOI: 10.1038/nature00767.Hon WC, Wilson MI, Harlos K, et al. Structural basis for the recognition of hydroxyproline in HIF-1α by pVHL. Nature. 2002, 417: 975-978. DOI: 10.1038/nature00767.
42、Semenza GL. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene. 2010, 29(5): 625-634. DOI: 10.1038/onc.2009.441.Semenza GL. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene. 2010, 29(5): 625-634. DOI: 10.1038/onc.2009.441.
43、Cummins EP,Berra E, Comerford KM, et al. Prolyl hydroxylase-1 negatively regulates IkappaB kinase-beta, giving insight into hypoxia-induced NFkappaB activity.
Proc Natl Acad Sci USA. 2006, 103(48): 18154-18159. DOI: 10.1073/pnas.0602235103.Cummins EP,Berra E, Comerford KM, et al. Prolyl hydroxylase-1 negatively regulates IkappaB kinase-beta, giving insight into hypoxia-induced NFkappaB activity.
Proc Natl Acad Sci USA. 2006, 103(48): 18154-18159. DOI: 10.1073/pnas.0602235103.
44、Kobayashi H, Gilbert V, Liu Q, et al. Myeloid cell�derived hypoxia-inducible factor attenuates inflammation in unilateral ureteral obstruction-induced kidney injury.
J Immunol. 2012, 188(10): 5106-5115. DOI: 10.4049/jimmunol.1103377.Kobayashi H, Gilbert V, Liu Q, et al. Myeloid cell�derived hypoxia-inducible factor attenuates inflammation in unilateral ureteral obstruction-induced kidney injury.
J Immunol. 2012, 188(10): 5106-5115. DOI: 10.4049/jimmunol.1103377.
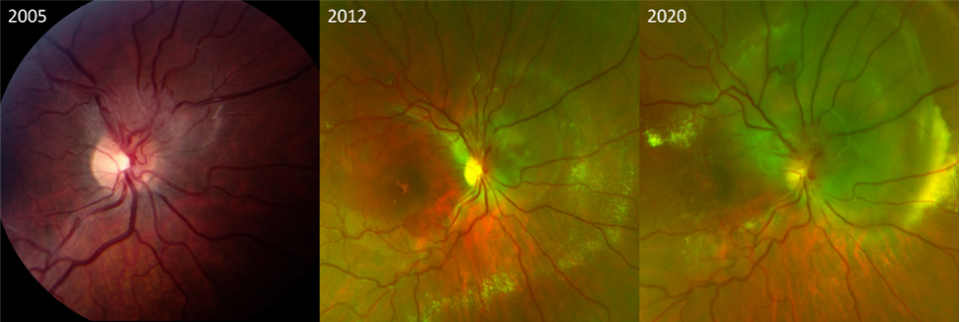
45、Toy BC, Agrón E, Nigam D, et al. Longitudinal analysis of retinal hemangioblastomatosis and visual function in ocular von Hippel-Lindau disease. Ophthalmology. 2012,
119(12): 2622-2630. DOI: 10.1016/j.ophtha.2012.06.026.Toy BC, Agrón E, Nigam D, et al. Longitudinal analysis of retinal hemangioblastomatosis and visual function in ocular von Hippel-Lindau disease. Ophthalmology. 2012,
119(12): 2622-2630. DOI: 10.1016/j.ophtha.2012.06.026.
46、Dahr SS, Cusick M, Rodriguez-Coleman H, et al. Intravitreal anti-vascular endothelial growth factor therapy with pegaptanib for advanced von Hippel-Lindau disease
of the retina. Retina. 2007, 27(2): 150-158. DOI: 10.1097/IAE.0b013e318030a290.Dahr SS, Cusick M, Rodriguez-Coleman H, et al. Intravitreal anti-vascular endothelial growth factor therapy with pegaptanib for advanced von Hippel-Lindau disease
of the retina. Retina. 2007, 27(2): 150-158. DOI: 10.1097/IAE.0b013e318030a290.
47、Kaelin WG. Molecular basis of the VHL hereditary cancer syndrome. Nat Rev Cancer. 2002, 2: 673-682. DOI: 10.1038/nrc885.Kaelin WG. Molecular basis of the VHL hereditary cancer syndrome. Nat Rev Cancer. 2002, 2: 673-682. DOI: 10.1038/nrc885.
48、Connolly DT, Heuvelman DM, Nelson R, et al. Tumor vascular permeability factor stimulates endothelial cell growth and angiogenesis. J ClinInvest. 1989, 84(5): 1470-1478. DOI: 10.1172/JCI114322.Connolly DT, Heuvelman DM, Nelson R, et al. Tumor vascular permeability factor stimulates endothelial cell growth and angiogenesis. J ClinInvest. 1989, 84(5): 1470-1478. DOI: 10.1172/JCI114322.
49、Wong WT, Liang KJ, Hammel K, et al. Intravitreal ranibizumab the rapy for retinal capillary hemangioblastoma related to von Hippel-Lindau disease. Ophthalmology. 2008, 115(11): 1957-1964. DOI: 10.1016/j.ophtha.2008.04.033Wong WT, Liang KJ, Hammel K, et al. Intravitreal ranibizumab the rapy for retinal capillary hemangioblastoma related to von Hippel-Lindau disease. Ophthalmology. 2008, 115(11): 1957-1964. DOI: 10.1016/j.ophtha.2008.04.033
50、Rini BI. Sunitinib. Expert Opin Pharmacother. 2007, 8(14): 2359-2369. DOI:10.1517/14656566.8.14.2359.Rini BI. Sunitinib. Expert Opin Pharmacother. 2007, 8(14): 2359-2369. DOI:10.1517/14656566.8.14.2359.
51、Knickelbein JE, Jacobs-El N, Wong WT, et al. Systemic sunitinib malate treatment for advanced juxtapapillary retinal hemangioblastomas associated with von hippel-lindau disease. Ophthalmol Retina. 2017, 1(3): 181-187. DOI: 10.1016/j.oret.2016.10.007.Knickelbein JE, Jacobs-El N, Wong WT, et al. Systemic sunitinib malate treatment for advanced juxtapapillary retinal hemangioblastomas associated with von hippel-lindau disease. Ophthalmol Retina. 2017, 1(3): 181-187. DOI: 10.1016/j.oret.2016.10.007.
52、Jonasch E, Donskov F, Iliopoulos O, et al. Belzutifan for renal cell carcinoma in von hippel-lindau disease. N Engl J Med. 2021, 385(22): 2036-2046. DOI: 10.1056/NEJMoa2103425.Jonasch E, Donskov F, Iliopoulos O, et al. Belzutifan for renal cell carcinoma in von hippel-lindau disease. N Engl J Med. 2021, 385(22): 2036-2046. DOI: 10.1056/NEJMoa2103425.
53、Wiley HE, Srinivasan R, Maranchie JK, et al. Oral hypoxia-inducible factor 2α inhibitor belzutifan in ocular von hippel-lindau disease: subgroup analysis of the single-arm phase 2 LITESPARK-004 study. Ophthalmology. 2024, 131(11): 1324-1332.DOI:10.1016/j.ophtha.2024.05.024.Wiley HE, Srinivasan R, Maranchie JK, et al. Oral hypoxia-inducible factor 2α inhibitor belzutifan in ocular von hippel-lindau disease: subgroup analysis of the single-arm phase 2 LITESPARK-004 study. Ophthalmology. 2024, 131(11): 1324-1332.DOI:10.1016/j.ophtha.2024.05.024.