1、Kolli S, Bojic S, Ghareeb AE, et al. The role of nerve growth factor in maintaining proliferative capacity, colony-forming efficiency, and the limbal stem cell phenotype. Stem Cells. 2019, 37(1): 139-149. DOI: 10.1002/stem.2921. Kolli S, Bojic S, Ghareeb AE, et al. The role of nerve growth factor in maintaining proliferative capacity, colony-forming efficiency, and the limbal stem cell phenotype. Stem Cells. 2019, 37(1): 139-149. DOI: 10.1002/stem.2921.
2、Notara M, Lentzsch A, Coroneo M, et al. The role of limbal epithelial stem cells in regulating corneal (lymph)angiogenic privilege and the micromilieu of the limbal niche following UV exposure. Stem Cells Int. 2018, 2018: 8620172. DOI: 10.1155/2018/8620172. Notara M, Lentzsch A, Coroneo M, et al. The role of limbal epithelial stem cells in regulating corneal (lymph)angiogenic privilege and the micromilieu of the limbal niche following UV exposure. Stem Cells Int. 2018, 2018: 8620172. DOI: 10.1155/2018/8620172.
3、Moreno IY, Parsaie A, Gesteira TF, et al. Characterization of the limbal epithelial stem cell niche. Invest Ophthalmol Vis Sci. 2023, 64(13): 48. DOI: 10.1167/iovs.64.13.48. Moreno IY, Parsaie A, Gesteira TF, et al. Characterization of the limbal epithelial stem cell niche. Invest Ophthalmol Vis Sci. 2023, 64(13): 48. DOI: 10.1167/iovs.64.13.48.
4、Chuephanich P, Supiyaphun C, Aravena C, et al. Characterization of the corneal subbasal nerve plexus in limbal stem cell deficiency. Cornea. 2017, 36(3): 347-352. DOI: 10.1097/ico.0000000000001092. Chuephanich P, Supiyaphun C, Aravena C, et al. Characterization of the corneal subbasal nerve plexus in limbal stem cell deficiency. Cornea. 2017, 36(3): 347-352. DOI: 10.1097/ico.0000000000001092.
5、DelMonte DW, Kim T. Anatomy and physiology of the cornea. J Cataract Refract Surg. 2011, 37(3): 588-598. DOI: 10.1016/j.jcrs.2010.12.037.DelMonte DW, Kim T. Anatomy and physiology of the cornea. J Cataract Refract Surg. 2011, 37(3): 588-598. DOI: 10.1016/j.jcrs.2010.12.037.
6、Bonnet C, González S, Roberts JS, et al. Human limbal epithelial stem cell regulation, bioengineering and function. Prog Retin Eye Res. 2021, 85: 100956. DOI: 10.1016/j.preteyeres.2021.100956. Bonnet C, González S, Roberts JS, et al. Human limbal epithelial stem cell regulation, bioengineering and function. Prog Retin Eye Res. 2021, 85: 100956. DOI: 10.1016/j.preteyeres.2021.100956.
7、Li M, Huang H, Li L, et al. Core transcription regulatory circuitry orchestrates corneal epithelial homeostasis. Nat Commun. 2021, 12: 420. DOI: 10.1038/s41467-020-20713-z. Li M, Huang H, Li L, et al. Core transcription regulatory circuitry orchestrates corneal epithelial homeostasis. Nat Commun. 2021, 12: 420. DOI: 10.1038/s41467-020-20713-z.
8、Altshuler A, Amitai-Lange A, Tarazi N, et al. Discrete limbal epithelial stem cell populations mediate corneal homeostasis and wound healing. Cell Stem Cell. 2021, 28(7): 1248-1261.e8. DOI: 10.1016/j.stem.2021.04.003.Altshuler A, Amitai-Lange A, Tarazi N, et al. Discrete limbal epithelial stem cell populations mediate corneal homeostasis and wound healing. Cell Stem Cell. 2021, 28(7): 1248-1261.e8. DOI: 10.1016/j.stem.2021.04.003.
9、Song Z, Chen B, Tsai CH, et al. Differentiation trajectory of limbal stem and progenitor cells under normal homeostasis and upon corneal wounding. Cells. 2022, 11(13): 1983. DOI: 10.3390/cells11131983. Song Z, Chen B, Tsai CH, et al. Differentiation trajectory of limbal stem and progenitor cells under normal homeostasis and upon corneal wounding. Cells. 2022, 11(13): 1983. DOI: 10.3390/cells11131983.
10、Majo F, Rochat A, Nicolas M, et al. Oligopotent stem cells are distributed throughout the mammalian ocular surface. Nature. 2008, 456: 250-254. DOI: 10.1038/nature07406.Majo F, Rochat A, Nicolas M, et al. Oligopotent stem cells are distributed throughout the mammalian ocular surface. Nature. 2008, 456: 250-254. DOI: 10.1038/nature07406.
11、Moshirfar M, Masud M, Harvey DH, et al. The multifold etiologies of limbal stem cell deficiency: a comprehensive review on the etiologies and additional treatment options for limbal stem cell deficiency. J Clin Med. 2023, 12(13): 4418. DOI: 10.3390/jcm12134418. Moshirfar M, Masud M, Harvey DH, et al. The multifold etiologies of limbal stem cell deficiency: a comprehensive review on the etiologies and additional treatment options for limbal stem cell deficiency. J Clin Med. 2023, 12(13): 4418. DOI: 10.3390/jcm12134418.
12、Verma S, Lin X, Coulson-Thomas VJ. The potential reversible transition between stem cells and transient-amplifying cells: the limbal epithelial stem cell perspective. Cells. 2024, 13(9): 748. DOI: 10.3390/cells13090748. Verma S, Lin X, Coulson-Thomas VJ. The potential reversible transition between stem cells and transient-amplifying cells: the limbal epithelial stem cell perspective. Cells. 2024, 13(9): 748. DOI: 10.3390/cells13090748.
13、 Galindo S, de la Mata A, López-Paniagua M, et al. Subconjunctival injection of mesenchymal stem cells for corneal failure due to limbal stem cell deficiency: state of the art. Stem Cell Res Ther. 2021, 12(1): 60. DOI: 10.1186/s13287-020-02129-0. Galindo S, de la Mata A, López-Paniagua M, et al. Subconjunctival injection of mesenchymal stem cells for corneal failure due to limbal stem cell deficiency: state of the art. Stem Cell Res Ther. 2021, 12(1): 60. DOI: 10.1186/s13287-020-02129-0.
14、Mei H, Gonzalez S, Deng SX. Extracellular matrix is an important component of limbal stem cell niche. J Funct Biomater. 2012, 3(4): 879-894. DOI: 10.3390/jfb3040879. Mei H, Gonzalez S, Deng SX. Extracellular matrix is an important component of limbal stem cell niche. J Funct Biomater. 2012, 3(4): 879-894. DOI: 10.3390/jfb3040879.
15、Okumura Y, Inomata T, Fujimoto K, et al. Biological effects of stored platelet-rich plasma eye-drops in corneal wound healing. Br J Ophthalmol. 2023, 108(1): 37-44. DOI: 10.1136/bjo-2022-322068. Okumura Y, Inomata T, Fujimoto K, et al. Biological effects of stored platelet-rich plasma eye-drops in corneal wound healing. Br J Ophthalmol. 2023, 108(1): 37-44. DOI: 10.1136/bjo-2022-322068.
16、Chen J, Chen P, Backman LJ, et al. Ciliary neurotrophic factor promotes the migration of corneal epithelial stem/progenitor cells by up-regulation of MMPs through the phosphorylation of Akt. Sci Rep. 2016, 6: 25870. DOI: 10.1038/srep25870. Chen J, Chen P, Backman LJ, et al. Ciliary neurotrophic factor promotes the migration of corneal epithelial stem/progenitor cells by up-regulation of MMPs through the phosphorylation of Akt. Sci Rep. 2016, 6: 25870. DOI: 10.1038/srep25870.
17、Chen J, Lan J, Liu D, et al. Ascorbic acid promotes the stemness of corneal epithelial stem/progenitor cells and accelerates epithelial wound healing in the cornea. Stem Cells Transl Med. 2017, 6(5): 1356-1365. DOI: 10.1002/sctm.16-0441. Chen J, Lan J, Liu D, et al. Ascorbic acid promotes the stemness of corneal epithelial stem/progenitor cells and accelerates epithelial wound healing in the cornea. Stem Cells Transl Med. 2017, 6(5): 1356-1365. DOI: 10.1002/sctm.16-0441.
18、Eslani M, Putra I, Shen X, et al. Cornea-derived mesenchymal stromal cells therapeutically modulate macrophage immunophenotype and angiogenic function. Stem Cells. 2018, 36(5): 775-784. DOI: 10.1002/stem.2781. Eslani M, Putra I, Shen X, et al. Cornea-derived mesenchymal stromal cells therapeutically modulate macrophage immunophenotype and angiogenic function. Stem Cells. 2018, 36(5): 775-784. DOI: 10.1002/stem.2781.
19、Volatier T, Cursiefen C, Notara M. Current advances in corneal stromal stem cell biology and therapeutic applications. Cells. 2024, 13(2): 163. DOI: 10.3390/cells13020163.Volatier T, Cursiefen C, Notara M. Current advances in corneal stromal stem cell biology and therapeutic applications. Cells. 2024, 13(2): 163. DOI: 10.3390/cells13020163.
20、Huang S, Kuri P, Aubert Y, et al. Lgr6 marks epidermal stem cells with a nerve-dependent role in wound re-epithelialization. Cell Stem Cell. 2021, 28(9): 1582-1596.e6. DOI: 10.1016/j.stem.2021.05.007. Huang S, Kuri P, Aubert Y, et al. Lgr6 marks epidermal stem cells with a nerve-dependent role in wound re-epithelialization. Cell Stem Cell. 2021, 28(9): 1582-1596.e6. DOI: 10.1016/j.stem.2021.05.007.
21、Al-Aqaba MA, Anis FS, Mohammed I, et al. Nerve terminals at the human corneoscleral limbus. Br J Ophthalmol. 2018, 102(4): 556-561. DOI: 10.1136/bjophthalmol-2017-311146. Al-Aqaba MA, Anis FS, Mohammed I, et al. Nerve terminals at the human corneoscleral limbus. Br J Ophthalmol. 2018, 102(4): 556-561. DOI: 10.1136/bjophthalmol-2017-311146.
22、Al-Aqaba MA, Dhillon VK, et al. Corneal nerves in health and disease. Prog Retin Eye Res. 2019, 73: 100762. DOI: 10.1016/j.preteyeres.2019.05.003.Al-Aqaba MA, Dhillon VK, et al. Corneal nerves in health and disease. Prog Retin Eye Res. 2019, 73: 100762. DOI: 10.1016/j.preteyeres.2019.05.003.
23、Caro-Magdaleno M, Alfaro-Juárez A, Montero-Iruzubieta J, et al. In vivo confocal microscopy indicates an inverse relationship between the sub-basal corneal plexus and the conjunctivalisation in patients with limbal stem cell deficiency. Br J Ophthalmol. 2019, 103(3): 327-331. DOI: 10.1136/bjophthalmol-2017-311693.Caro-Magdaleno M, Alfaro-Juárez A, Montero-Iruzubieta J, et al. In vivo confocal microscopy indicates an inverse relationship between the sub-basal corneal plexus and the conjunctivalisation in patients with limbal stem cell deficiency. Br J Ophthalmol. 2019, 103(3): 327-331. DOI: 10.1136/bjophthalmol-2017-311693.
24、Khilji M, Tanveer S, Khan FZ, et al. Neurotrophic Keratopathy and Topical Insulin Therapy: A Case Report. Cureus. 2023, 15(9): e46242. DOI: 10.7759/cureus.46242.Khilji M, Tanveer S, Khan FZ, et al. Neurotrophic Keratopathy and Topical Insulin Therapy: A Case Report. Cureus. 2023, 15(9): e46242. DOI: 10.7759/cureus.46242.
25、NaPier E, Camacho M, McDevitt TF, et al. Neurotrophic keratopathy: current challenges and future prospects. Ann Med. 2022, 54(1): 666-673. DOI: 10.1080/07853890.2022.2045035. NaPier E, Camacho M, McDevitt TF, et al. Neurotrophic keratopathy: current challenges and future prospects. Ann Med. 2022, 54(1): 666-673. DOI: 10.1080/07853890.2022.2045035.
26、 Surico PL, Narimatsu A, Forouzanfar K, et al. Effects of diabetes mellitus on corneal immune cell activation and the development of keratopathy. Cells. 2024, 13(6): 532. DOI: 10.3390/cells13060532. Surico PL, Narimatsu A, Forouzanfar K, et al. Effects of diabetes mellitus on corneal immune cell activation and the development of keratopathy. Cells. 2024, 13(6): 532. DOI: 10.3390/cells13060532.
27、Bhattacharya P, Edwards K, Harkin D, et al. Central corneal basal cell density and nerve parameters in ocular surface disease and limbal stem cell deficiency: a review and meta-analysis. Br J Ophthalmol. 2020, 104(12): 1633-1639. DOI: 10.1136/bjophthalmol-2019-315231. Bhattacharya P, Edwards K, Harkin D, et al. Central corneal basal cell density and nerve parameters in ocular surface disease and limbal stem cell deficiency: a review and meta-analysis. Br J Ophthalmol. 2020, 104(12): 1633-1639. DOI: 10.1136/bjophthalmol-2019-315231.
28、Bonnet%20C%2C%20et%20al.%20Cell%20Morphology%20as%20an%20In%20Vivo%20Parameter%20for%20the%20Diagnosis%20of%20Limbal%20Stem%20Cell%20Deficiency.%20Cornea.%202022%2C%2041(8)%3A995-1001.%20DOI%3A%2010.1097%2FICO.0000000000002955.%C2%A0Bonnet%20C%2C%20et%20al.%20Cell%20Morphology%20as%20an%20In%20Vivo%20Parameter%20for%20the%20Diagnosis%20of%20Limbal%20Stem%20Cell%20Deficiency.%20Cornea.%202022%2C%2041(8)%3A995-1001.%20DOI%3A%2010.1097%2FICO.0000000000002955.%C2%A0
29、Wang LY, Wei ZY, Cao K, et al. In vivo confocal microscopic characteristics of limbal stem cell deficiency. Zhonghua Yan Ke Za Zhi. 2020, 56(6): 447-455. DOI: 10.3760/cma.j.cn112142-20191221-00660. Wang LY, Wei ZY, Cao K, et al. In vivo confocal microscopic characteristics of limbal stem cell deficiency. Zhonghua Yan Ke Za Zhi. 2020, 56(6): 447-455. DOI: 10.3760/cma.j.cn112142-20191221-00660.
30、Li Y, Ma X, Li J, et al. Corneal denervation causes epithelial apoptosis through inhibiting NAD+ biosynthesis. Invest Ophthalmol Vis Sci. 2019, 60(10): 3538-3546. DOI: 10.1167/iovs.19-26909. Li Y, Ma X, Li J, et al. Corneal denervation causes epithelial apoptosis through inhibiting NAD+ biosynthesis. Invest Ophthalmol Vis Sci. 2019, 60(10): 3538-3546. DOI: 10.1167/iovs.19-26909.
31、Ueno H, Ferrari G, Hattori T, et al. Dependence of corneal stem/progenitor cells on ocular surface innervation. Invest Ophthalmol Vis Sci. 2012, 53(2): 867-872. DOI: 10.1167/iovs.11-8438.Ueno H, Ferrari G, Hattori T, et al. Dependence of corneal stem/progenitor cells on ocular surface innervation. Invest Ophthalmol Vis Sci. 2012, 53(2): 867-872. DOI: 10.1167/iovs.11-8438.
32、Yazdanpanah G, Jabbehdari S, Djalilian AR. Limbal and corneal epithelial homeostasis. Curr Opin Ophthalmol. 2017, 28(4): 348-354. DOI: 10.1097/icu.0000000000000378.Yazdanpanah G, Jabbehdari S, Djalilian AR. Limbal and corneal epithelial homeostasis. Curr Opin Ophthalmol. 2017, 28(4): 348-354. DOI: 10.1097/icu.0000000000000378.
33、Amin S, Jalilian E, Katz E, et al. The limbal niche and regenerative strategies. Vision (Basel). 2021, 5(4): 43. DOI: 10.3390/vision5040043.Amin S, Jalilian E, Katz E, et al. The limbal niche and regenerative strategies. Vision (Basel). 2021, 5(4): 43. DOI: 10.3390/vision5040043.
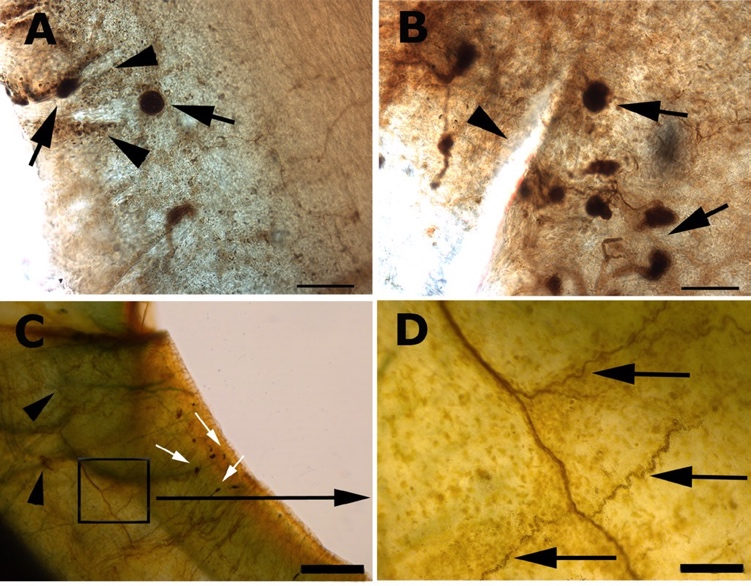
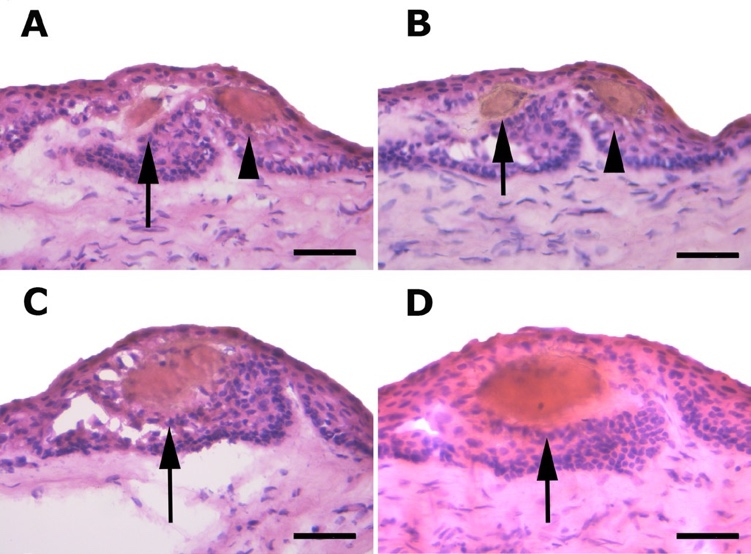
34、 Grieve K, Ghoubay D, Georgeon C, et al. Three-dimensional structure of the mammalian limbal stem cell niche. Exp Eye Res, 2015, 140: 75-84. DOI: 10.1016/j.exer.2015.08.003. Grieve K, Ghoubay D, Georgeon C, et al. Three-dimensional structure of the mammalian limbal stem cell niche. Exp Eye Res, 2015, 140: 75-84. DOI: 10.1016/j.exer.2015.08.003.
35、Sun D, Shi WY, Dou SQ. Single-cell RNA sequencing in cornea research: Insights into limbal stem cells and their niche regulation. World J Stem Cells. 2023, 15(5): 466-475. DOI: 10.4252/wjsc.v15.i5.466.Sun D, Shi WY, Dou SQ. Single-cell RNA sequencing in cornea research: Insights into limbal stem cells and their niche regulation. World J Stem Cells. 2023, 15(5): 466-475. DOI: 10.4252/wjsc.v15.i5.466.
36、Yazdanpanah G, Haq Z, Kang K, et al. Strategies for reconstructing the limbal stem cell niche. Ocul Surf. 2019, 17(2): 230-240. DOI: 10.1016/j.jtos.2019.01.002.Yazdanpanah G, Haq Z, Kang K, et al. Strategies for reconstructing the limbal stem cell niche. Ocul Surf. 2019, 17(2): 230-240. DOI: 10.1016/j.jtos.2019.01.002.
37、Medeiros CS, Santhiago MR. Corneal nerves anatomy, function, injury and regeneration. Exp Eye Res. 2020, 200: 108243. DOI: 10.1016/j.exer.2020.108243.Medeiros CS, Santhiago MR. Corneal nerves anatomy, function, injury and regeneration. Exp Eye Res. 2020, 200: 108243. DOI: 10.1016/j.exer.2020.108243.
38、Yang AY, Chow J, Liu J. Corneal Innervation and Sensation: The Eye and Beyond. Yale J Biol Med. 2018, 91(1): 13-21.Yang AY, Chow J, Liu J. Corneal Innervation and Sensation: The Eye and Beyond. Yale J Biol Med. 2018, 91(1): 13-21.
39、Stepp%20MA%2C%20Pal-Ghosh%20S%2C%20Downie%20LE%2C%20et%20al.%20Corneal%20epithelial%20%E2%80%9Cneuromas%E2%80%9D%3A%20a%20case%20of%20mistaken%20identity%3F.%20Cornea.%202020%2C%2039(7)%3A%20930-934.%20DOI%3A%2010.1097%2Fico.0000000000002294.%20Stepp%20MA%2C%20Pal-Ghosh%20S%2C%20Downie%20LE%2C%20et%20al.%20Corneal%20epithelial%20%E2%80%9Cneuromas%E2%80%9D%3A%20a%20case%20of%20mistaken%20identity%3F.%20Cornea.%202020%2C%2039(7)%3A%20930-934.%20DOI%3A%2010.1097%2Fico.0000000000002294.%20
40、Wang C, Fu T, Xia C, et al. Changes in mouse corneal epithelial innervation with age. Invest Ophthalmol Vis Sci. 2012, 53(8): 5077. DOI: 10.1167/iovs.12-9704. Wang C, Fu T, Xia C, et al. Changes in mouse corneal epithelial innervation with age. Invest Ophthalmol Vis Sci. 2012, 53(8): 5077. DOI: 10.1167/iovs.12-9704.
41、Tuck H, Park M, Carnell M, et al. Neuronal-epithelial cell alignment: a determinant of health and disease status of the cornea. Ocul Surf. 2021, 21: 257-270. DOI: 10.1016/j.jtos.2021.03.007. Tuck H, Park M, Carnell M, et al. Neuronal-epithelial cell alignment: a determinant of health and disease status of the cornea. Ocul Surf. 2021, 21: 257-270. DOI: 10.1016/j.jtos.2021.03.007.
42、Al-Aqaba MA, Fares U, Suleman H, et al. Architecture and distribution of human corneal nerves. Br J Ophthalmol. 2010, 94(6): 784-789. DOI: 10.1136/bjo.2009.173799. Al-Aqaba MA, Fares U, Suleman H, et al. Architecture and distribution of human corneal nerves. Br J Ophthalmol. 2010, 94(6): 784-789. DOI: 10.1136/bjo.2009.173799.
43、Badian RA, Lagali N. The inferocentral whorl region and its directional patterns in the corneal sub-basal nerve plexus: a review. Exp Eye Res. 2024, 244: 109926. DOI: 10.1016/j.exer.2024.109926. Badian RA, Lagali N. The inferocentral whorl region and its directional patterns in the corneal sub-basal nerve plexus: a review. Exp Eye Res. 2024, 244: 109926. DOI: 10.1016/j.exer.2024.109926.
44、Stache N, Sterenczak KA, Sperlich K, et al. Assessment of dynamic corneal nerve changes using static landmarks by in vivo large-area confocal microscopy: a longitudinal proof-of-concept study. Quant Imaging Med Surg. 2022, 12(10): 4734-4746. DOI: 10.21037/qims-22-15. Stache N, Sterenczak KA, Sperlich K, et al. Assessment of dynamic corneal nerve changes using static landmarks by in vivo large-area confocal microscopy: a longitudinal proof-of-concept study. Quant Imaging Med Surg. 2022, 12(10): 4734-4746. DOI: 10.21037/qims-22-15.
45、Bhattacharya S, Mukherjee A, Pisano S, et al. The biophysical property of the limbal niche maintains stemness through YAP. Cell Death Differ. 2023, 30(6): 1601-1614. DOI: 10.1038/s41418-023-01156-7. Bhattacharya S, Mukherjee A, Pisano S, et al. The biophysical property of the limbal niche maintains stemness through YAP. Cell Death Differ. 2023, 30(6): 1601-1614. DOI: 10.1038/s41418-023-01156-7.
46、 Collinson JM, Chanas SA, Hill RE, et al. Corneal development, limbal stem cell function, and corneal epithelial cell migration in the Pax6(+ /-) mouse. Invest Ophthalmol Vis Sci. 2004, 45(4): 1101-1108. DOI: 10.1167/iovs.03-1118. Collinson JM, Chanas SA, Hill RE, et al. Corneal development, limbal stem cell function, and corneal epithelial cell migration in the Pax6(+ /-) mouse. Invest Ophthalmol Vis Sci. 2004, 45(4): 1101-1108. DOI: 10.1167/iovs.03-1118.
47、Collinson JM, Morris L, Reid AI, et al. Clonal analysis of patterns of growth, stem cell activity, and cell movement during the development and maintenance of the murine corneal epithelium. Dev Dyn. 2002, 224(4): 432-440. DOI: 10.1002/dvdy.10124.Collinson JM, Morris L, Reid AI, et al. Clonal analysis of patterns of growth, stem cell activity, and cell movement during the development and maintenance of the murine corneal epithelium. Dev Dyn. 2002, 224(4): 432-440. DOI: 10.1002/dvdy.10124.
48、Marfurt CF, Cox J, Deek S, et al. Anatomy of the human corneal innervation. Exp Eye Res. 2010, 90(4): 478-492. DOI: 10.1016/j.exer.2009.12.010. Marfurt CF, Cox J, Deek S, et al. Anatomy of the human corneal innervation. Exp Eye Res. 2010, 90(4): 478-492. DOI: 10.1016/j.exer.2009.12.010.
49、Marfurt CF, Ellis LC. Immunohistochemical localization of tyrosine hydroxylase in corneal nerves. J Comp Neurol. 1993, 336(4): 517-531. DOI: 10.1002/cne.903360405. Marfurt CF, Ellis LC. Immunohistochemical localization of tyrosine hydroxylase in corneal nerves. J Comp Neurol. 1993, 336(4): 517-531. DOI: 10.1002/cne.903360405.
50、Singh RB, Naderi A, Cho W, et al. Modulating the tachykinin: Role of substance P and neurokinin receptor expression in ocular surface disorders. Ocul Surf. 2022, 25: 142-153. DOI: 10.1016/j.jtos.2022.06.007. Singh RB, Naderi A, Cho W, et al. Modulating the tachykinin: Role of substance P and neurokinin receptor expression in ocular surface disorders. Ocul Surf. 2022, 25: 142-153. DOI: 10.1016/j.jtos.2022.06.007.
51、%20S%C5%82oniecka%20M%2C%20Le%20Roux%20S%2C%20Zhou%20Q%2C%20et%20al.%20Substance%20P%20enhances%20keratocyte%20migration%20and%20neutrophil%20recruitment%20through%20interleukin-8.%20Mol%20Pharmacol.%202016%2C%2089(2)%3A%20215-225.%20DOI%3A%2010.1124%2Fmol.115.101014.%20%20S%C5%82oniecka%20M%2C%20Le%20Roux%20S%2C%20Zhou%20Q%2C%20et%20al.%20Substance%20P%20enhances%20keratocyte%20migration%20and%20neutrophil%20recruitment%20through%20interleukin-8.%20Mol%20Pharmacol.%202016%2C%2089(2)%3A%20215-225.%20DOI%3A%2010.1124%2Fmol.115.101014.%20
52、Lasagni Vitar R, Triani F, Barbariga M, et al. Substance P/neurokinin-1 receptor pathway blockade ameliorates limbal stem cell deficiency by modulating mTOR pathway and preventing cell senescence. Stem Cell Rep. 2022, 17(4): 849-863. DOI: 10.1016/j.stemcr.2022.02.012. Lasagni Vitar R, Triani F, Barbariga M, et al. Substance P/neurokinin-1 receptor pathway blockade ameliorates limbal stem cell deficiency by modulating mTOR pathway and preventing cell senescence. Stem Cell Rep. 2022, 17(4): 849-863. DOI: 10.1016/j.stemcr.2022.02.012.
53、Wang Y, Gao G, Wu Y, et al. S100A4 silencing facilitates corneal wound healing after alkali burns by promoting autophagy via blocking the PI3K/Akt/mTOR signaling pathway. Invest Ophthalmol Vis Sci. 2020, 61(11): 19. DOI: 10.1167/iovs.61.11.19. Wang Y, Gao G, Wu Y, et al. S100A4 silencing facilitates corneal wound healing after alkali burns by promoting autophagy via blocking the PI3K/Akt/mTOR signaling pathway. Invest Ophthalmol Vis Sci. 2020, 61(11): 19. DOI: 10.1167/iovs.61.11.19.
54、Bignami F, Rama P, Ferrari G. Substance P and its inhibition in ocular inflammation. Curr Drug Targets. 2016, 17(11): 1265-1274. DOI: 10.2174/1389450116666151019100216. Bignami F, Rama P, Ferrari G. Substance P and its inhibition in ocular inflammation. Curr Drug Targets. 2016, 17(11): 1265-1274. DOI: 10.2174/1389450116666151019100216.
55、Kowtharapu BS, Murín R, Jünemann AGM, et al. Role of corneal stromal cells on epithelial cell function during wound healing. Int J Mol Sci. 2018, 19(2): E464. DOI: 10.3390/ijms19020464.Kowtharapu BS, Murín R, Jünemann AGM, et al. Role of corneal stromal cells on epithelial cell function during wound healing. Int J Mol Sci. 2018, 19(2): E464. DOI: 10.3390/ijms19020464.
56、Yang L, Di G, Qi X, et al. Substance P promotes diabetic corneal epithelial wound healing through molecular mechanisms mediated via the neurokinin-1 receptor. Diabetes. 2014, 63(12): 4262-4274. DOI: 10.2337/db14-0163.Yang L, Di G, Qi X, et al. Substance P promotes diabetic corneal epithelial wound healing through molecular mechanisms mediated via the neurokinin-1 receptor. Diabetes. 2014, 63(12): 4262-4274. DOI: 10.2337/db14-0163.
57、Redkiewicz P. The regenerative potential of substance P. Int J Mol Sci. 2022, 23(2): 750. DOI: 10.3390/ijms23020750. Redkiewicz P. The regenerative potential of substance P. Int J Mol Sci. 2022, 23(2): 750. DOI: 10.3390/ijms23020750.
58、Lasagni Vitar RM, Fonteyne P, Chaabane L, et al. A hypothalamic-controlled neural reflex promotes corneal inflammation. Invest Ophthalmol Vis Sci. 2021, 62(13): 21. DOI: 10.1167/iovs.62.13.21.Lasagni Vitar RM, Fonteyne P, Chaabane L, et al. A hypothalamic-controlled neural reflex promotes corneal inflammation. Invest Ophthalmol Vis Sci. 2021, 62(13): 21. DOI: 10.1167/iovs.62.13.21.
59、Sun J, Ramnath RD, Tamizhselvi R, et al. Role of protein kinase C and phosphoinositide 3-kinase-Akt in substance P-induced proinflammatory pathways in mouse macrophages. FASEB J. 2009, 23(4): 997-1010. DOI: 10.1096/fj.08-121756. Sun J, Ramnath RD, Tamizhselvi R, et al. Role of protein kinase C and phosphoinositide 3-kinase-Akt in substance P-induced proinflammatory pathways in mouse macrophages. FASEB J. 2009, 23(4): 997-1010. DOI: 10.1096/fj.08-121756.
60、Gaddipati S, Rao P, Jerome AD, et al. Loss of neurokinin-1 receptor alters ocular surface homeostasis and promotes an early development of herpes stromal keratitis. J Immunol. 2016, 197(10): 4021-4033. DOI: 10.4049/jimmunol.1600836.Gaddipati S, Rao P, Jerome AD, et al. Loss of neurokinin-1 receptor alters ocular surface homeostasis and promotes an early development of herpes stromal keratitis. J Immunol. 2016, 197(10): 4021-4033. DOI: 10.4049/jimmunol.1600836.
61、Woronkowicz M, Roberts H, Skopiński P. The role of insulin-like growth factor (IGF) system in the corneal epithelium homeostasis-from limbal epithelial stem cells to therapeutic applications. Biology (Basel). 2024, 13(3): 144. DOI: 10.3390/biology13030144. Woronkowicz M, Roberts H, Skopiński P. The role of insulin-like growth factor (IGF) system in the corneal epithelium homeostasis-from limbal epithelial stem cells to therapeutic applications. Biology (Basel). 2024, 13(3): 144. DOI: 10.3390/biology13030144.
62、Yang L, Sui W, Li Y, et al. Substance P inhibits hyperosmotic stress-induced apoptosis in corneal epithelial cells through the mechanism of Akt activation and reactive oxygen species scavenging via the neurokinin-1 receptor. PLoS One. 2016, 11(2): e0149865. DOI: 10.1371/journal.pone.0149865. Yang L, Sui W, Li Y, et al. Substance P inhibits hyperosmotic stress-induced apoptosis in corneal epithelial cells through the mechanism of Akt activation and reactive oxygen species scavenging via the neurokinin-1 receptor. PLoS One. 2016, 11(2): e0149865. DOI: 10.1371/journal.pone.0149865.
63、Ko JA, Yanai R, Nishida T. Up-regulation of ZO-1 expression and barrier function in cultured human corneal epithelial cells by substance P. FEBS Lett. 2009, 583(12): 2148-2153. DOI: 10.1016/j.febslet.2009.05.010. Ko JA, Yanai R, Nishida T. Up-regulation of ZO-1 expression and barrier function in cultured human corneal epithelial cells by substance P. FEBS Lett. 2009, 583(12): 2148-2153. DOI: 10.1016/j.febslet.2009.05.010.
64、 Puri S, Kenyon BM, Hamrah P. Immunomodulatory role of neuropeptides in the cornea. Biomedicines. 2022, 10(8): 1985. DOI: 10.3390/biomedicines10081985. Puri S, Kenyon BM, Hamrah P. Immunomodulatory role of neuropeptides in the cornea. Biomedicines. 2022, 10(8): 1985. DOI: 10.3390/biomedicines10081985.
65、Aerts-Kaya F, et al. Neurological Regulation of the Bone Marrow Niche. Adv Exp Med Biol. 2020, 1212: 127-153. DOI: 10.1007/5584_2019_398 .Aerts-Kaya F, et al. Neurological Regulation of the Bone Marrow Niche. Adv Exp Med Biol. 2020, 1212: 127-153. DOI: 10.1007/5584_2019_398 .
66、Mu C, Hu Y, Hou Y, et al. Substance P-embedded multilayer on titanium substrates promotes local osseointegration via MSC recruitment. J Mater Chem B. 2020, 8(6): 1212-1222. DOI: 10.1039/c9tb01124b.Mu C, Hu Y, Hou Y, et al. Substance P-embedded multilayer on titanium substrates promotes local osseointegration via MSC recruitment. J Mater Chem B. 2020, 8(6): 1212-1222. DOI: 10.1039/c9tb01124b.
67、Jung J, Jeong J, Hong HS. Substance P improves MSC-mediated RPE regeneration by modulating PDGF-BB. Biochem Biophys Res Commun. 2019, 515(4): 524-530. DOI: 10.1016/j.bbrc.2019.05.186. Jung J, Jeong J, Hong HS. Substance P improves MSC-mediated RPE regeneration by modulating PDGF-BB. Biochem Biophys Res Commun. 2019, 515(4): 524-530. DOI: 10.1016/j.bbrc.2019.05.186.
68、Cheng P, Sun X, Yin D, et al. Nanog down-regulates the Wnt signaling pathway via β-catenin phosphorylation during epidermal stem cell proliferation and differentiation. Cell Biosci. 2015, 5: 5. DOI: 10.1186/2045-3701-5-5.Cheng P, Sun X, Yin D, et al. Nanog down-regulates the Wnt signaling pathway via β-catenin phosphorylation during epidermal stem cell proliferation and differentiation. Cell Biosci. 2015, 5: 5. DOI: 10.1186/2045-3701-5-5.
69、Yin M, Li C, Peng XD, et al. Expression and role of calcitonin gene-related peptide in mouse Aspergillus fumigatus keratitis. Int J Ophthalmol. 2019, 12(5): 697-704. DOI: 10.18240/ijo.2019.05.01.Yin M, Li C, Peng XD, et al. Expression and role of calcitonin gene-related peptide in mouse Aspergillus fumigatus keratitis. Int J Ophthalmol. 2019, 12(5): 697-704. DOI: 10.18240/ijo.2019.05.01.
70、Yuan K, et al. Sensory nerves promote corneal inflammation resolution via CGRP mediated transformation of macrophages to the M2 phenotype through the PI3K/AKT signaling pathway. Int Immunopharmacol. 2022, 102: 108426. DOI: 10.1016/j.intimp.2021.108426 .Yuan K, et al. Sensory nerves promote corneal inflammation resolution via CGRP mediated transformation of macrophages to the M2 phenotype through the PI3K/AKT signaling pathway. Int Immunopharmacol. 2022, 102: 108426. DOI: 10.1016/j.intimp.2021.108426 .
71、Mikulec AA, Tanelian DL. CGRP increases the rate of corneal re-epithelialization in an in vitro whole mount preparation. J Ocul Pharmacol Ther. 1996, 12(4): 417-423. DOI: 10.1089/jop.1996.12.417. Mikulec AA, Tanelian DL. CGRP increases the rate of corneal re-epithelialization in an in vitro whole mount preparation. J Ocul Pharmacol Ther. 1996, 12(4): 417-423. DOI: 10.1089/jop.1996.12.417.
72、Zhu S, Zidan A, Pang K, et al. Promotion of corneal angiogenesis by sensory neuron-derived calcitonin gene-related peptide. Exp Eye Res. 2022, 220: 109125. DOI: 10.1016/j.exer.2022.109125.Zhu S, Zidan A, Pang K, et al. Promotion of corneal angiogenesis by sensory neuron-derived calcitonin gene-related peptide. Exp Eye Res. 2022, 220: 109125. DOI: 10.1016/j.exer.2022.109125.
73、Kadar T, Dachir S, Cohen M, et al. Prolonged impairment of corneal innervation after exposure to sulfur mustard and its relation to the development of delayed limbal stem cell deficiency. Cornea. 2013, 32(4): e44-50. DOI: 10.1097/ico.0b013e318262e885. Kadar T, Dachir S, Cohen M, et al. Prolonged impairment of corneal innervation after exposure to sulfur mustard and its relation to the development of delayed limbal stem cell deficiency. Cornea. 2013, 32(4): e44-50. DOI: 10.1097/ico.0b013e318262e885.
74、Sullivan C, et al. Evidence for a phenotypic switch in corneal afferents after lacrimal gland excision. Exp Eye Res. 2022, 218: 109005. DOI: 10.1016/j.exer.2022.109005.Sullivan C, et al. Evidence for a phenotypic switch in corneal afferents after lacrimal gland excision. Exp Eye Res. 2022, 218: 109005. DOI: 10.1016/j.exer.2022.109005.
75、Diel RJ, Mehra D, Kardon R, et al. Photophobia: shared pathophysiology underlying dry eye disease, migraine and traumatic brain injury leading to central neuroplasticity of the trigeminothalamic pathway. Br J Ophthalmol. 2021, 105(6): 751-760. DOI: 10.1136/bjophthalmol-2020-316417.Diel RJ, Mehra D, Kardon R, et al. Photophobia: shared pathophysiology underlying dry eye disease, migraine and traumatic brain injury leading to central neuroplasticity of the trigeminothalamic pathway. Br J Ophthalmol. 2021, 105(6): 751-760. DOI: 10.1136/bjophthalmol-2020-316417.
76、Weirath NA, Haskell-Luevano C. Recommended tool compounds for the melanocortin receptor (MCR) G protein-coupled receptors (GPCRs). ACS Pharmacol Transl Sci. 2024, 7(9): 2706-2724. DOI: 10.1021/acsptsci.4c00129.Weirath NA, Haskell-Luevano C. Recommended tool compounds for the melanocortin receptor (MCR) G protein-coupled receptors (GPCRs). ACS Pharmacol Transl Sci. 2024, 7(9): 2706-2724. DOI: 10.1021/acsptsci.4c00129.
77、Chu C, Huang Y, Ru Y, et al. α-MSH ameliorates corneal surface dysfunction in scopolamine-induced dry eye rats and human corneal epithelial cells via enhancing EGFR expression. Exp Eye Res. 2021, 210: 108685. DOI: 10.1016/j.exer.2021.108685. Chu C, Huang Y, Ru Y, et al. α-MSH ameliorates corneal surface dysfunction in scopolamine-induced dry eye rats and human corneal epithelial cells via enhancing EGFR expression. Exp Eye Res. 2021, 210: 108685. DOI: 10.1016/j.exer.2021.108685.
78、Nohara K, Zhang Y, Waraich RS, et al. Early-life exposure to testosterone programs the hypothalamic melanocortin system. Endocrinology. 2011, 152(4): 1661-1669. DOI: 10.1210/en.2010-1288. Nohara K, Zhang Y, Waraich RS, et al. Early-life exposure to testosterone programs the hypothalamic melanocortin system. Endocrinology. 2011, 152(4): 1661-1669. DOI: 10.1210/en.2010-1288.
79、Daini E, Vandini E, Bodria M, et al. Melanocortin receptor agonist NDP-α-MSH improves cognitive deficits and microgliosis but not amyloidosis in advanced stages of AD progression in 5XFAD and 3xTg mice. Front Immunol. 2023, 13: 1082036. DOI: 10.3389/fimmu.2022.1082036. Daini E, Vandini E, Bodria M, et al. Melanocortin receptor agonist NDP-α-MSH improves cognitive deficits and microgliosis but not amyloidosis in advanced stages of AD progression in 5XFAD and 3xTg mice. Front Immunol. 2023, 13: 1082036. DOI: 10.3389/fimmu.2022.1082036.
80、Bock F, Onderka J, Braun G, et al. Identification of novel endogenous anti(lymph)angiogenic factors in the aqueous humor. Invest Ophthalmol Vis Sci. 2016, 57(15): 6554. DOI: 10.1167/iovs.15-18526. Bock F, Onderka J, Braun G, et al. Identification of novel endogenous anti(lymph)angiogenic factors in the aqueous humor. Invest Ophthalmol Vis Sci. 2016, 57(15): 6554. DOI: 10.1167/iovs.15-18526.
81、Li C, Wu M, Gu L, et al. α- MSH plays anti-inflammatory and anti-fungal role in Aspergillus fumigatus keratitis. Curr Eye Res. 2022, 47(3): 343-351. DOI: 10.1080/02713683.2021.2006235. Li C, Wu M, Gu L, et al. α- MSH plays anti-inflammatory and anti-fungal role in Aspergillus fumigatus keratitis. Curr Eye Res. 2022, 47(3): 343-351. DOI: 10.1080/02713683.2021.2006235.
82、Kistenmacher%20S%2C%20Schw%C3%A4mmle%20M%2C%20Martin%20G%2C%20et%20al.%20Enrichment%2C%20characterization%2C%20and%20proteomic%20profiling%20of%20small%20extracellular%20vesicles%20derived%20from%20human%20limbal%20mesenchymal%20stromal%20cells%20and%20melanocytes.%20Cells.%202024%2C%2013(7)%3A%20623.%20DOI%3A%2010.3390%2Fcells13070623.%20Kistenmacher%20S%2C%20Schw%C3%A4mmle%20M%2C%20Martin%20G%2C%20et%20al.%20Enrichment%2C%20characterization%2C%20and%20proteomic%20profiling%20of%20small%20extracellular%20vesicles%20derived%20from%20human%20limbal%20mesenchymal%20stromal%20cells%20and%20melanocytes.%20Cells.%202024%2C%2013(7)%3A%20623.%20DOI%3A%2010.3390%2Fcells13070623.%20
83、Dziasko MA, Tuft SJ, Daniels JT. Limbal melanocytes support limbal epithelial stem cells in 2D and 3D microenvironments. Exp Eye Res. 2015, 138: 70-79. DOI: 10.1016/j.exer.2015.06.026. Dziasko MA, Tuft SJ, Daniels JT. Limbal melanocytes support limbal epithelial stem cells in 2D and 3D microenvironments. Exp Eye Res. 2015, 138: 70-79. DOI: 10.1016/j.exer.2015.06.026.
84、 Li H, Hou L. Regulation of melanocyte stem cell behavior by the niche microenvironment. Pigment Cell Melanoma Res. 2018, 31(5): 556-569. DOI: 10.1111/pcmr.12701. Li H, Hou L. Regulation of melanocyte stem cell behavior by the niche microenvironment. Pigment Cell Melanoma Res. 2018, 31(5): 556-569. DOI: 10.1111/pcmr.12701.
85、Lu%C5%BEnik%20Marzidov%C5%A1ek%20Z%2C%20Blanco%20T%2C%20Sun%20Z%2C%20et%20al.%20The%20neuropeptide%20alpha-melanocyte%E2%80%93stimulating%20hormone%20is%20critical%20for%20corneal%20endothelial%20cell%20protection%20and%20graft%20survival%20after%20transplantation.%20Am%20J%20Pathol.%202022%2C%20192(2)%3A%20270-280.%20DOI%3A%2010.1016%2Fj.ajpath.2021.10.016.%20Lu%C5%BEnik%20Marzidov%C5%A1ek%20Z%2C%20Blanco%20T%2C%20Sun%20Z%2C%20et%20al.%20The%20neuropeptide%20alpha-melanocyte%E2%80%93stimulating%20hormone%20is%20critical%20for%20corneal%20endothelial%20cell%20protection%20and%20graft%20survival%20after%20transplantation.%20Am%20J%20Pathol.%202022%2C%20192(2)%3A%20270-280.%20DOI%3A%2010.1016%2Fj.ajpath.2021.10.016.%20
86、Mashimo M, Moriwaki Y, Misawa H, et al. Regulation of immune functions by non-neuronal acetylcholine (ACh) via muscarinic and nicotinic ACh receptors. Int J Mol Sci. 2021, 22(13): 6818. DOI: 10.3390/ijms22136818.Mashimo M, Moriwaki Y, Misawa H, et al. Regulation of immune functions by non-neuronal acetylcholine (ACh) via muscarinic and nicotinic ACh receptors. Int J Mol Sci. 2021, 22(13): 6818. DOI: 10.3390/ijms22136818.
87、S%C5%82oniecka%20M%2C%20Danielson%20P.%20Acetylcholine%20decreases%20formation%20of%20myofibroblasts%20and%20excessive%20extracellular%20matrix%20production%20in%20an%20in%20vitro%20human%20corneal%20fibrosis%20model.%20J%20Cell%20Mol%20Med.%202020%2C%2024(8)%3A%204850-4862.%20DOI%3A%2010.1111%2Fjcmm.15168.%20S%C5%82oniecka%20M%2C%20Danielson%20P.%20Acetylcholine%20decreases%20formation%20of%20myofibroblasts%20and%20excessive%20extracellular%20matrix%20production%20in%20an%20in%20vitro%20human%20corneal%20fibrosis%20model.%20J%20Cell%20Mol%20Med.%202020%2C%2024(8)%3A%204850-4862.%20DOI%3A%2010.1111%2Fjcmm.15168.%20
88、Kurzen H, Wessler I, Kirkpatrick CJ, et al. The non-neuronal cholinergic system of human skin. Horm Metab Res. 2007, 39(2): 125-135. DOI: 10.1055/s-2007-961816. Kurzen H, Wessler I, Kirkpatrick CJ, et al. The non-neuronal cholinergic system of human skin. Horm Metab Res. 2007, 39(2): 125-135. DOI: 10.1055/s-2007-961816.
89、Takahashi T. Roles of nAChR and Wnt signaling in intestinal stem cell function and inflammation. Int Immunopharmacol. 2020, 81: 106260. DOI: 10.1016/j.intimp.2020.106260.Takahashi T. Roles of nAChR and Wnt signaling in intestinal stem cell function and inflammation. Int Immunopharmacol. 2020, 81: 106260. DOI: 10.1016/j.intimp.2020.106260.
90、Tracey KJ. Reflex control of immunity. Nat Rev Immunol. 2009, 9(6): 418-428. DOI: 10.1038/nri2566. Tracey KJ. Reflex control of immunity. Nat Rev Immunol. 2009, 9(6): 418-428. DOI: 10.1038/nri2566.
91、Grando SA, Pittelkow MR, Schallreuter KU. Adrenergic and cholinergic control in the biology of epidermis: physiological and clinical significance. J Investig Dermatol. 2006, 126(9): 1948-1965. DOI: 10.1038/sj.jid.5700151. Grando SA, Pittelkow MR, Schallreuter KU. Adrenergic and cholinergic control in the biology of epidermis: physiological and clinical significance. J Investig Dermatol. 2006, 126(9): 1948-1965. DOI: 10.1038/sj.jid.5700151.
92、S%C5%82oniecka%20M%2C%20Backman%20LJ%2C%20Danielson%20P.%20Acetylcholine%20enhances%20keratocyte%20proliferation%20through%20muscarinic%20receptor%20activation.%20Int%20Immunopharmacol.%202015%2C%2029(1)%3A%2057-62.%20DOI%3A%2010.1016%2Fj.intimp.2015.05.039.%20S%C5%82oniecka%20M%2C%20Backman%20LJ%2C%20Danielson%20P.%20Acetylcholine%20enhances%20keratocyte%20proliferation%20through%20muscarinic%20receptor%20activation.%20Int%20Immunopharmacol.%202015%2C%2029(1)%3A%2057-62.%20DOI%3A%2010.1016%2Fj.intimp.2015.05.039.%20
93、Pflugfelder SC, Cao A, Galor A, et al. Nicotinic acetylcholine receptor stimulation: a new approach for stimulating tear secretion in dry eye disease. Ocul Surf. 2022, 25: 58-64. DOI: 10.1016/j.jtos.2022.05.001.Pflugfelder SC, Cao A, Galor A, et al. Nicotinic acetylcholine receptor stimulation: a new approach for stimulating tear secretion in dry eye disease. Ocul Surf. 2022, 25: 58-64. DOI: 10.1016/j.jtos.2022.05.001.
94、Wirta D, Vollmer P, Paauw J, et al. Efficacy and safety of OC-01 (varenicline solution) nasal spray on signs and symptoms of dry eye disease the ONSET-2 phase 3 randomized trial. Ophthalmology. 2022, 129(4): 379-387. DOI: 10.1016/j.ophtha.2021.11.004. Wirta D, Vollmer P, Paauw J, et al. Efficacy and safety of OC-01 (varenicline solution) nasal spray on signs and symptoms of dry eye disease the ONSET-2 phase 3 randomized trial. Ophthalmology. 2022, 129(4): 379-387. DOI: 10.1016/j.ophtha.2021.11.004.
95、Musayeva A, Jiang S, Ruan Y, et al. Aged mice devoid of the M3 muscarinic acetylcholine receptor develop mild dry eye disease. Int J Mol Sci. 2021, 22(11): 6133. DOI: 10.3390/ijms22116133. Musayeva A, Jiang S, Ruan Y, et al. Aged mice devoid of the M3 muscarinic acetylcholine receptor develop mild dry eye disease. Int J Mol Sci. 2021, 22(11): 6133. DOI: 10.3390/ijms22116133.
96、Grando SA. Connections of nicotine to cancer. Nat Rev Cancer. 2014, 14: 419-429. DOI: 10.1038/nrc3725.Grando SA. Connections of nicotine to cancer. Nat Rev Cancer. 2014, 14: 419-429. DOI: 10.1038/nrc3725.
97、Chernyavsky AI, Galitovskiy V, Grando SA. Molecular mechanisms of synergy of corneal muscarinic and nicotinic acetylcholine receptors in upregulation of E-cadherin expression. Int Immunopharmacol. 2015, 29(1): 15-20. DOI: 10.1016/j.intimp.2015.04.036.Chernyavsky AI, Galitovskiy V, Grando SA. Molecular mechanisms of synergy of corneal muscarinic and nicotinic acetylcholine receptors in upregulation of E-cadherin expression. Int Immunopharmacol. 2015, 29(1): 15-20. DOI: 10.1016/j.intimp.2015.04.036.
98、 Xue Y, et al. The mouse autonomic nervous system modulates inflammation and epithelial renewal after corneal abrasion through the activation of distinct local macrophages. Mucosal Immunol. 2018, 11(5):1496-1511. DOI: 10.1038/s41385-018-0031-6. Xue Y, et al. The mouse autonomic nervous system modulates inflammation and epithelial renewal after corneal abrasion through the activation of distinct local macrophages. Mucosal Immunol. 2018, 11(5):1496-1511. DOI: 10.1038/s41385-018-0031-6.
99、Chernyavsky AI, Galitovskiy V, Shchepotin IB, et al. The acetylcholine signaling network of corneal epithelium and its role in regulation of random and directional migration of corneal epithelial cells. Investig Ophthalmol Vis Sci. 2014, 55(10): 6921-6933. DOI: 10.1167/iovs.14-14667. Chernyavsky AI, Galitovskiy V, Shchepotin IB, et al. The acetylcholine signaling network of corneal epithelium and its role in regulation of random and directional migration of corneal epithelial cells. Investig Ophthalmol Vis Sci. 2014, 55(10): 6921-6933. DOI: 10.1167/iovs.14-14667.
100、Maestroni GJM. Adrenergic modulation of hematopoiesis. J Neuroimmune Pharmacol. 2020, 15(1): 82-92. DOI: 10.1007/s11481-019-09840-7. Maestroni GJM. Adrenergic modulation of hematopoiesis. J Neuroimmune Pharmacol. 2020, 15(1): 82-92. DOI: 10.1007/s11481-019-09840-7.
101、Figueira L, Ferreira C, Janeiro C, et al. Concentration gradient of noradrenaline from the periphery to the centre of the cornea - A clue to its origin. Exp Eye Res. 2018, 168: 107-114. DOI: 10.1016/j.exer.2018.01.008. Figueira L, Ferreira C, Janeiro C, et al. Concentration gradient of noradrenaline from the periphery to the centre of the cornea - A clue to its origin. Exp Eye Res. 2018, 168: 107-114. DOI: 10.1016/j.exer.2018.01.008.
102、 Li J, Ma X, Zhao L, et al. Extended contact lens wear promotes corneal norepinephrine secretion and pseudomonas aeruginosa infection in mice. Invest Ophthalmol Vis Sci. 2020, 61(4): 17. DOI: 10.1167/iovs.61.4.17. Li J, Ma X, Zhao L, et al. Extended contact lens wear promotes corneal norepinephrine secretion and pseudomonas aeruginosa infection in mice. Invest Ophthalmol Vis Sci. 2020, 61(4): 17. DOI: 10.1167/iovs.61.4.17.
103、Ma X, Wang Q, Song F, et al. Corneal epithelial injury-induced norepinephrine promotes Pseudomonas aeruginosa keratitis. Exp Eye Res. 2020, 195: 108048. DOI: 10.1016/j.exer.2020.108048. Ma X, Wang Q, Song F, et al. Corneal epithelial injury-induced norepinephrine promotes Pseudomonas aeruginosa keratitis. Exp Eye Res. 2020, 195: 108048. DOI: 10.1016/j.exer.2020.108048.
104、Lee H, Lee JH, Hong S, et al. Transplantation of human corneal limbal epithelial cell sheet harvested on synthesized carboxymethyl cellulose and dopamine in a limbal stem cell deficiency. J Tissue Eng Regen Med. 2021, 15(2): 139-149. DOI: 10.1002/term.3159. Lee H, Lee JH, Hong S, et al. Transplantation of human corneal limbal epithelial cell sheet harvested on synthesized carboxymethyl cellulose and dopamine in a limbal stem cell deficiency. J Tissue Eng Regen Med. 2021, 15(2): 139-149. DOI: 10.1002/term.3159.
105、Figueira L, Janeiro C, Ferreirinha F, et al. Regulation of corneal noradrenaline release and topography of sympathetic innervation: Functional implications for adrenergic mechanisms in the human cornea. Exp Eye Res. 2018, 174: 121-132. DOI: 10.1016/j.exer.2018.05.023. Figueira L, Janeiro C, Ferreirinha F, et al. Regulation of corneal noradrenaline release and topography of sympathetic innervation: Functional implications for adrenergic mechanisms in the human cornea. Exp Eye Res. 2018, 174: 121-132. DOI: 10.1016/j.exer.2018.05.023.
106、Ghoghawala SY, Mannis MJ, Pullar CE, et al. Beta2-adrenergic receptor signaling mediates corneal epithelial wound repair. Invest Ophthalmol Vis Sci. 2008, 49(5): 1857-1863. DOI: 10.1167/iovs.07-0925.Ghoghawala SY, Mannis MJ, Pullar CE, et al. Beta2-adrenergic receptor signaling mediates corneal epithelial wound repair. Invest Ophthalmol Vis Sci. 2008, 49(5): 1857-1863. DOI: 10.1167/iovs.07-0925.
107、Grueb M, Bartz-Schmidt KU, Rohrbach JM. Adrenergic regulation of cAMP/protein kinase A pathway in corneal epithelium and endothelium. Ophthalmic Res. 2008, 40(6): 322-328. DOI: 10.1159/000150446.Grueb M, Bartz-Schmidt KU, Rohrbach JM. Adrenergic regulation of cAMP/protein kinase A pathway in corneal epithelium and endothelium. Ophthalmic Res. 2008, 40(6): 322-328. DOI: 10.1159/000150446.
108、 Zhang X, Muddana S, Kumar SR, et al. Topical pergolide enhance corneal nerve regrowth following induced corneal abrasion. Invest Ophthalmol Vis Sci. 2020, 61(1): 4. DOI: 10.1167/iovs.61.1.4. Zhang X, Muddana S, Kumar SR, et al. Topical pergolide enhance corneal nerve regrowth following induced corneal abrasion. Invest Ophthalmol Vis Sci. 2020, 61(1): 4. DOI: 10.1167/iovs.61.1.4.
109、Cavallotti C, Pescosolido N, Artico M, et al. Localization of dopamine receptors in the rabbit cornea. Cornea. 1999, 18(6): 721-728. DOI: 10.1097/00003226-199911000-00016. Cavallotti C, Pescosolido N, Artico M, et al. Localization of dopamine receptors in the rabbit cornea. Cornea. 1999, 18(6): 721-728. DOI: 10.1097/00003226-199911000-00016.
110、Rose-John S. Interleukin-6 family cytokines. Cold Spring Harb Perspect Biol. 2018, 10(2): a028415. DOI: 10.1101/cshperspect.a028415. Rose-John S. Interleukin-6 family cytokines. Cold Spring Harb Perspect Biol. 2018, 10(2): a028415. DOI: 10.1101/cshperspect.a028415.
111、Oh B, Wu YW, Swaminathan V, et al. Modulating the electrical and mechanical microenvironment to guide neuronal stem cell differentiation. Adv Sci. 2021, 8(7): 2002112. DOI: 10.1002/advs.202002112. Oh B, Wu YW, Swaminathan V, et al. Modulating the electrical and mechanical microenvironment to guide neuronal stem cell differentiation. Adv Sci. 2021, 8(7): 2002112. DOI: 10.1002/advs.202002112.
112、Reichard M, Hovakimyan M, Guthoff RF, et al. In vivo visualisation of murine corneal nerve fibre regeneration in response to ciliary neurotrophic factor. Exp Eye Res. 2014, 120: 20-27. DOI: 10.1016/j.exer.2013.12.015. Reichard M, Hovakimyan M, Guthoff RF, et al. In vivo visualisation of murine corneal nerve fibre regeneration in response to ciliary neurotrophic factor. Exp Eye Res. 2014, 120: 20-27. DOI: 10.1016/j.exer.2013.12.015.
113、Qi H, Chuang EY, Yoon KC, et al. Patterned expression of neurotrophic factors and receptors in human limbal and corneal regions. Mol Vis. 2007, 13: 1934-1941. Qi H, Chuang EY, Yoon KC, et al. Patterned expression of neurotrophic factors and receptors in human limbal and corneal regions. Mol Vis. 2007, 13: 1934-1941.
114、Chung ES, Lee KH, Kim M, et al. Expression of neurotrophic factors and their receptors in keratoconic cornea. Curr Eye Res. 2013, 38(7): 743-750. DOI: 10.3109/02713683.2013.774421. Chung ES, Lee KH, Kim M, et al. Expression of neurotrophic factors and their receptors in keratoconic cornea. Curr Eye Res. 2013, 38(7): 743-750. DOI: 10.3109/02713683.2013.774421.
115、Zhou Q, Chen P, Di G, et al. Ciliary neurotrophic factor promotes the activation of corneal epithelial stem/progenitor cells and accelerates corneal epithelial wound healing. Stem Cells. 2015, 33(5): 1566-1576. DOI: 10.1002/stem.1942.Zhou Q, Chen P, Di G, et al. Ciliary neurotrophic factor promotes the activation of corneal epithelial stem/progenitor cells and accelerates corneal epithelial wound healing. Stem Cells. 2015, 33(5): 1566-1576. DOI: 10.1002/stem.1942.
116、Levi-Montalcini R. The nerve growth factor 35 years later. Science. 1987, 237(4819): 1154-1162. DOI: 10.1126/science.3306916.Levi-Montalcini R. The nerve growth factor 35 years later. Science. 1987, 237(4819): 1154-1162. DOI: 10.1126/science.3306916.
117、Chen H, Zhang J, Dai Y, et al. Nerve growth factor inhibits TLR3-induced inflammatory cascades in human corneal epithelial cells. J Inflamm (Lond). 2019, 16: 27. DOI: 10.1186/s12950-019-0232-0. Chen H, Zhang J, Dai Y, et al. Nerve growth factor inhibits TLR3-induced inflammatory cascades in human corneal epithelial cells. J Inflamm (Lond). 2019, 16: 27. DOI: 10.1186/s12950-019-0232-0.
118、 Lambiase A, Manni L, Bonini S, et al. Nerve growth factor promotes corneal healing: structural, biochemical, and molecular analyses of rat and human corneas. Invest Ophthalmol Vis Sci. 2000, 41(5):1063-9. Lambiase A, Manni L, Bonini S, et al. Nerve growth factor promotes corneal healing: structural, biochemical, and molecular analyses of rat and human corneas. Invest Ophthalmol Vis Sci. 2000, 41(5):1063-9.
119、Aloe L, Tirassa P, Lambiase A. The topical application of nerve growth factor as a pharmacological tool for human corneal and skin ulcers. Pharmacol Res. 2008, 57(4): 253-258. DOI: 10.1016/j.phrs.2008.01.010. Aloe L, Tirassa P, Lambiase A. The topical application of nerve growth factor as a pharmacological tool for human corneal and skin ulcers. Pharmacol Res. 2008, 57(4): 253-258. DOI: 10.1016/j.phrs.2008.01.010.
120、Fink DM, Connor AL, Kelley PM, et al. Nerve growth factor regulates neurolymphatic remodeling during corneal inflammation and resolution. PLoS One. 2014, 9(11): e112737. DOI: 10.1371/journal.pone.0112737. Fink DM, Connor AL, Kelley PM, et al. Nerve growth factor regulates neurolymphatic remodeling during corneal inflammation and resolution. PLoS One. 2014, 9(11): e112737. DOI: 10.1371/journal.pone.0112737.
121、Park JH, Kang SS, Kim JY, et al. Nerve growth factor attenuates apoptosis and inflammation in the diabetic cornea. Invest Ophthalmol Vis Sci. 2016, 57(15): 6767. DOI: 10.1167/iovs.16-19747. Park JH, Kang SS, Kim JY, et al. Nerve growth factor attenuates apoptosis and inflammation in the diabetic cornea. Invest Ophthalmol Vis Sci. 2016, 57(15): 6767. DOI: 10.1167/iovs.16-19747.
122、 Di G, Qi X, Zhao X, et al. Corneal epithelium-derived neurotrophic factors promote nerve regeneration. Invest Ophthalmol Vis Sci. 2017, 58(11): 4695-4702. DOI: 10.1167/iovs.16-21372. Di G, Qi X, Zhao X, et al. Corneal epithelium-derived neurotrophic factors promote nerve regeneration. Invest Ophthalmol Vis Sci. 2017, 58(11): 4695-4702. DOI: 10.1167/iovs.16-21372.
123、 Qi H, Li DQ, Shine HD, et al. Nerve growth factor and its receptor TrkA serve as potential markers for human corneal epithelial progenitor cells. Exp Eye Res. 2008, 86(1): 34-40. DOI: 10.1016/j.exer.2007.09.003. Qi H, Li DQ, Shine HD, et al. Nerve growth factor and its receptor TrkA serve as potential markers for human corneal epithelial progenitor cells. Exp Eye Res. 2008, 86(1): 34-40. DOI: 10.1016/j.exer.2007.09.003.
124、Pedrotti E, Bonacci E, Chierego C, et al. Eight months follow-up of corneal nerves and sensitivity after treatment with cenegermin for neurotrophic keratopathy. Orphanet J Rare Dis. 2022, 17(1): 63. DOI: 10.1186/s13023-022-02237-5. Pedrotti E, Bonacci E, Chierego C, et al. Eight months follow-up of corneal nerves and sensitivity after treatment with cenegermin for neurotrophic keratopathy. Orphanet J Rare Dis. 2022, 17(1): 63. DOI: 10.1186/s13023-022-02237-5.
125、Hong%20J%2C%20et%20al.%20NGF%20promotes%20cell%20cycle%20progression%20by%20regulating%20D-type%20cyclins%20via%20PI3K%2FAkt%20and%20MAPK%2FErk%20activation%20in%20human%20corneal%20epithelial%20cells.%20Mol%20Vis.%202012%2C%2018%3A%20758-764.%C2%A0%20Hong%20J%2C%20et%20al.%20NGF%20promotes%20cell%20cycle%20progression%20by%20regulating%20D-type%20cyclins%20via%20PI3K%2FAkt%20and%20MAPK%2FErk%20activation%20in%20human%20corneal%20epithelial%20cells.%20Mol%20Vis.%202012%2C%2018%3A%20758-764.%C2%A0%20
126、Ting DSJ. Re: bonini et al. phase 2 randomized, double-masked, vehicle-controlled trial of recombinant human nerve growth factor for neurotrophic keratitis (ophthalmology. 2018;125: 1332-1343). Ophthalmology. 2019, 126(2): e14-e15. DOI: 10.1016/j.ophtha.2018.09.017. Ting DSJ. Re: bonini et al. phase 2 randomized, double-masked, vehicle-controlled trial of recombinant human nerve growth factor for neurotrophic keratitis (ophthalmology. 2018;125: 1332-1343). Ophthalmology. 2019, 126(2): e14-e15. DOI: 10.1016/j.ophtha.2018.09.017.
127、Pedrotti E, Bonetto J, Cozzini T, et al. Cenegermin in pediatric neurotrophic keratopathy. Cornea. 2019, 38(11): 1450-1452. DOI: 10.1097/ico.0000000000002112.Pedrotti E, Bonetto J, Cozzini T, et al. Cenegermin in pediatric neurotrophic keratopathy. Cornea. 2019, 38(11): 1450-1452. DOI: 10.1097/ico.0000000000002112.
128、Compagnoni C, Zelli V, Bianchi A, et al. microRNAs expression in response to rhNGF in epithelial corneal cells: focus on neurotrophin signaling pathway. Int J Mol Sci. 2022, 23(7): 3597. DOI: 10.3390/ijms23073597. Compagnoni C, Zelli V, Bianchi A, et al. microRNAs expression in response to rhNGF in epithelial corneal cells: focus on neurotrophin signaling pathway. Int J Mol Sci. 2022, 23(7): 3597. DOI: 10.3390/ijms23073597.
129、Kalaimani L, Devarajan B, Namperumalsamy VP, et al. Hsa-miR-143-3p inhibits Wnt-β-catenin and MAPK signaling in human corneal epithelial stem cells. Sci Rep. 2022, 12(1): 11432. DOI: 10.1038/s41598-022-15263-x.Kalaimani L, Devarajan B, Namperumalsamy VP, et al. Hsa-miR-143-3p inhibits Wnt-β-catenin and MAPK signaling in human corneal epithelial stem cells. Sci Rep. 2022, 12(1): 11432. DOI: 10.1038/s41598-022-15263-x.