Prog Retin Eye Res | Professor Xiulan Zhang's Team from ZOC Published Comprehensive Review on Distinguishing Optic Neuropathy in High Myopia and Glaucoma
发布时间:2024-12-19 浏览:1594
Editorial Office
On January 21, 2024, Professor Xiulan Zhang's team, with Zhongshan Ophthalmic Center (ZOC) , Sun Yat-sen University as the first affiliation, published a comprehensive review titled "Optic Neuropathy in High Myopia: Glaucoma or High Myopia or Both?" in the top ophthalmology journal "Progress in Retinal and Eye Research" (Figure 1). The review extensively elucidates the similarities and differences in imaging structure and function between optic neuropathy in high myopia and glaucoma, providing important insights for the early diagnosis, screening, and treatment of glaucoma in highly myopic patients.
Figure 1 Comprehensive review from Zhongshan Ophthalmic Center, Sun Yat-sen University in "Progress in Retinal and Eye Research"
High myopia is a widespread blinding eye disease affecting 163 million people worldwide (2.7% of the population) in 2000, projected to reach 938 million by 2050. It poses a significant risk for glaucoma, with high myopia patients having a 2.92 to 7.3 times higher risk compared to the general population. Distinguishing optic neuropathy between these conditions is challenging. Based on a comprehensive literature review, this article summarizes the characteristics of high myopia and glaucoma in terms of fundus photography, optical coherence tomography (OCT), optical coherence tomography angiography (OCTA), visual fields, and other structural and functional aspects, aiding early differentiation and standardized management for high myopia and glaucoma patients.
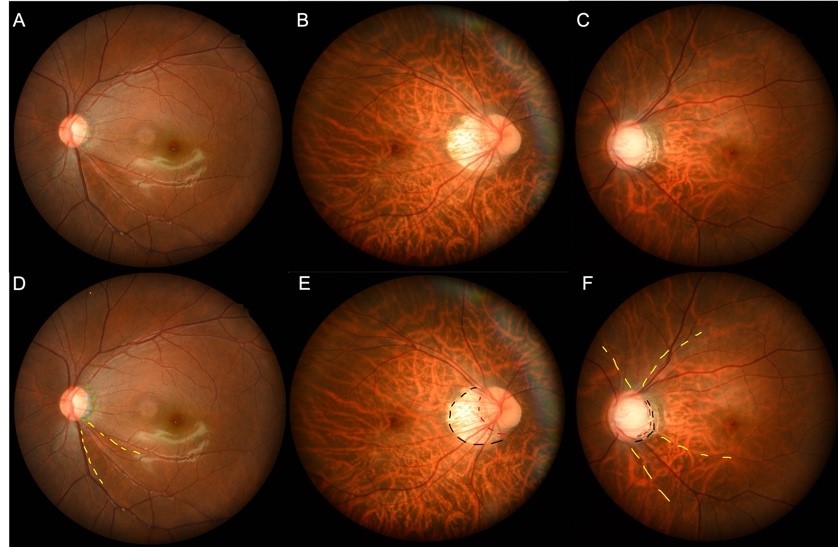
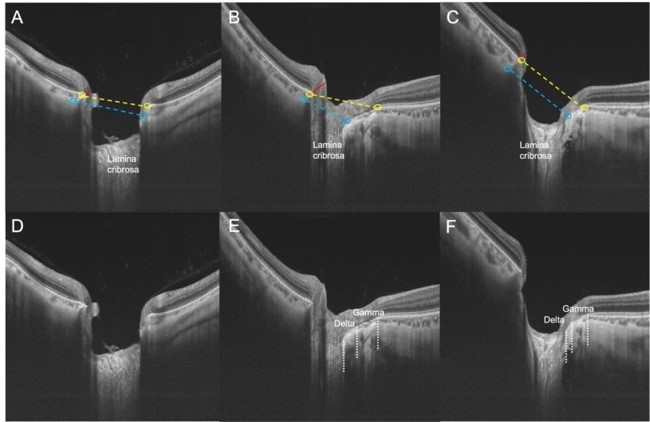
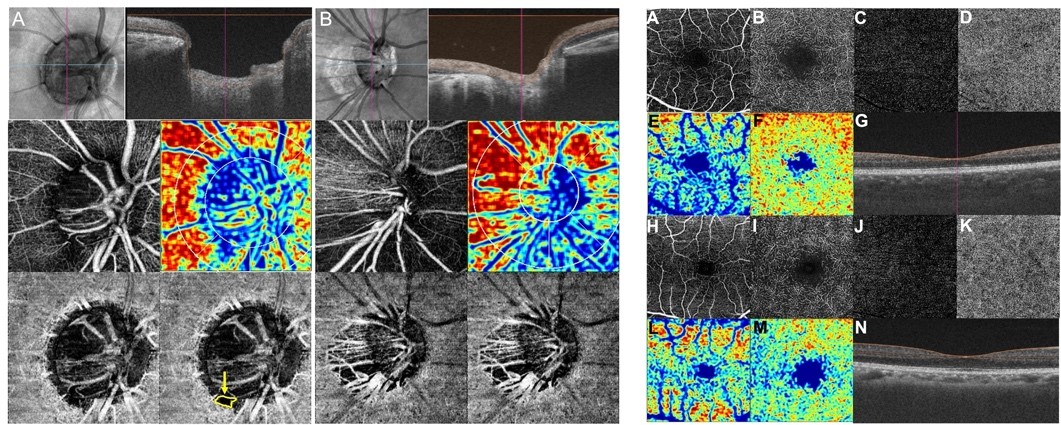
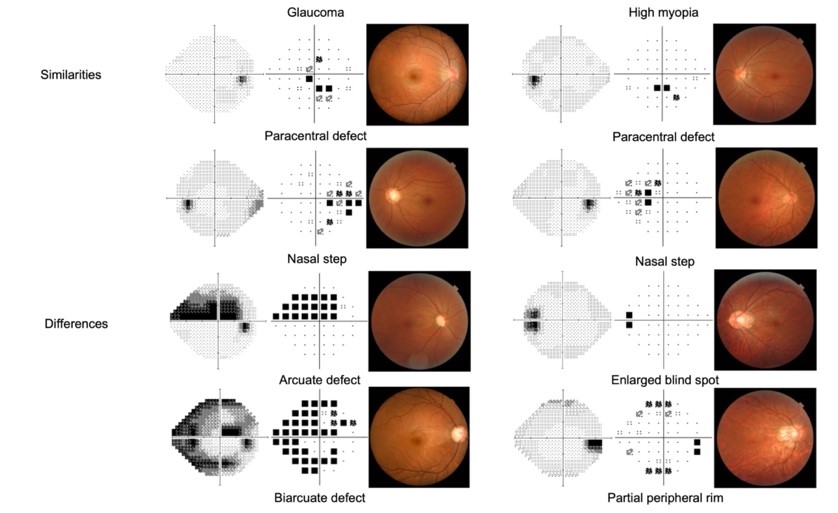
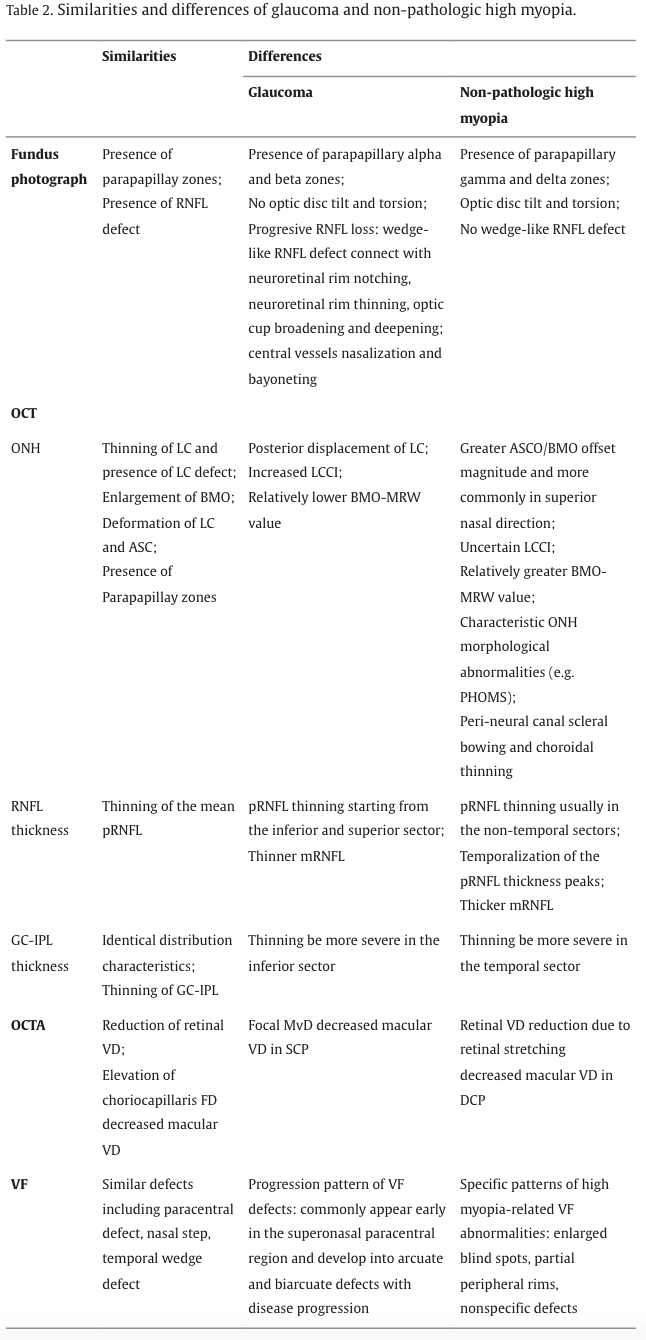
This article provides a comprehensive review of the similarities and differences between high myopia and glaucoma in fundus photography, OCT, OCTA, and visual field examinations. Fundus photography: Both conditions exhibit changes in optic disc morphology and peripapillary areas, including thinning of the retinal nerve fiber layer (RNFL) and disc margin, but high myopia is characterized by distinct Gamma and Delta zones, whereas glaucoma shows typical disc rim and progressive RNFL wedge defects (Figure 2). OCT: Various optic disc morphological parameters, such as cup-to-disc ratio and Bruch's membrane opening (BMO) size, were compared, along with the distribution of RNFL and ganglion cell-inner plexiform layer (GC-IPL) thickness (Figure 3). OCTA: The characteristics of peripapillary and macular microvascular flow were described. Microvascular density loss in high myopia mainly occurs in the deep retinal capillary plexus, while in glaucoma, it primarily affects the superficial retinal capillary plexus (Figure 4). Visual field: Eight common visual field defects in high myopia and glaucoma were summarized. Both conditions can exhibit paracentral scotomas, nasal step, temporal wedge defects, and vertical step defects. High myopia is characterized by enlarged blind spots and partial peripheral defects, while glaucoma presents characteristic arcuate and annular defects (Figure 5).
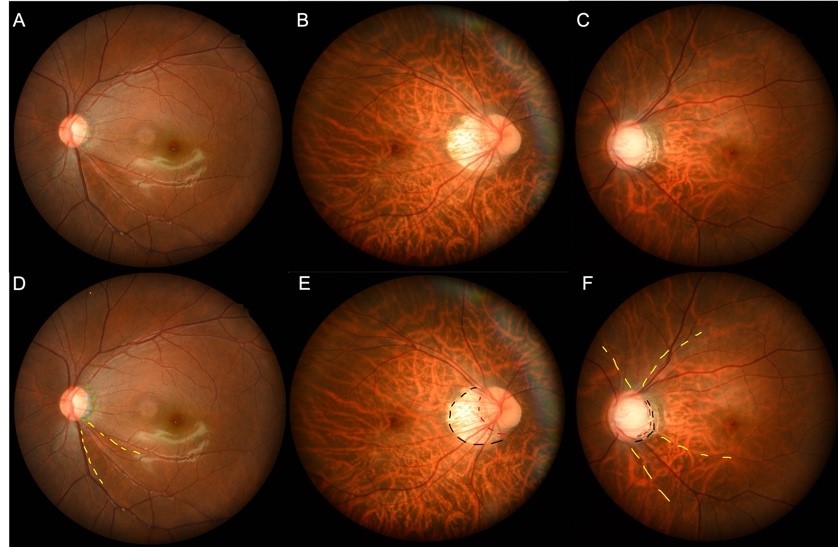
Figure 2 Distinctive alterations features of high myopia and glaucoma in fundus photography
A, D: glaucoma B, E: high myopia C, F: high myopia with glaucoma
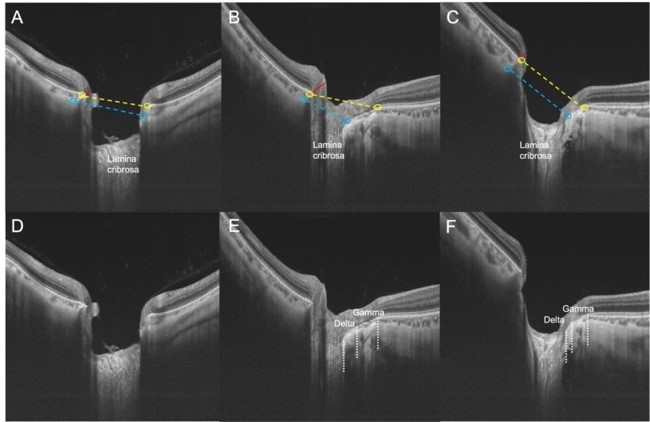
Figure 3 Distinctive alterations features of high myopia and glaucoma in optical coherence tomography (OCT)
A, D: glaucoma B, E: high myopia C, F: high myopia with glaucoma
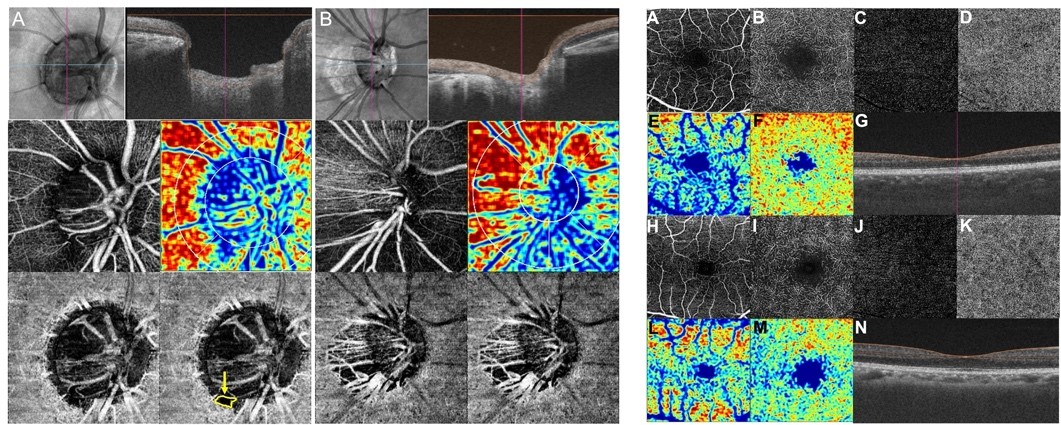
Figure 4 Distinctive alterations features of high myopia and glaucoma in optical coherence tomography angiography (OCTA)
Left (peripapillary OCTA) A: glaucoma B: high myopia;
Right (macular OCTA) A-G: glaucoma H-N: high myopia
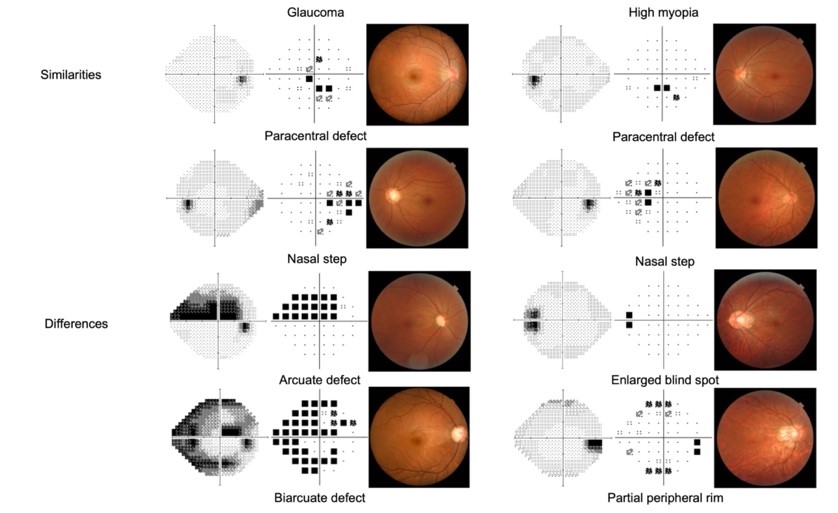
Figure 5 Distinctive alterations features of high myopia and glaucoma in visual field
This review further summarizes the key similarities and differences in the structural and functional characteristics of high myopia and glaucoma (Figure 6), emphasizes the importance of establishing standardized imaging and related normative databases for high myopia, and highlights the insufficient international understanding of optic neuropathy associated with high myopia. It suggests the need for longitudinal research and international consensus to enhance the understanding of the diseases.
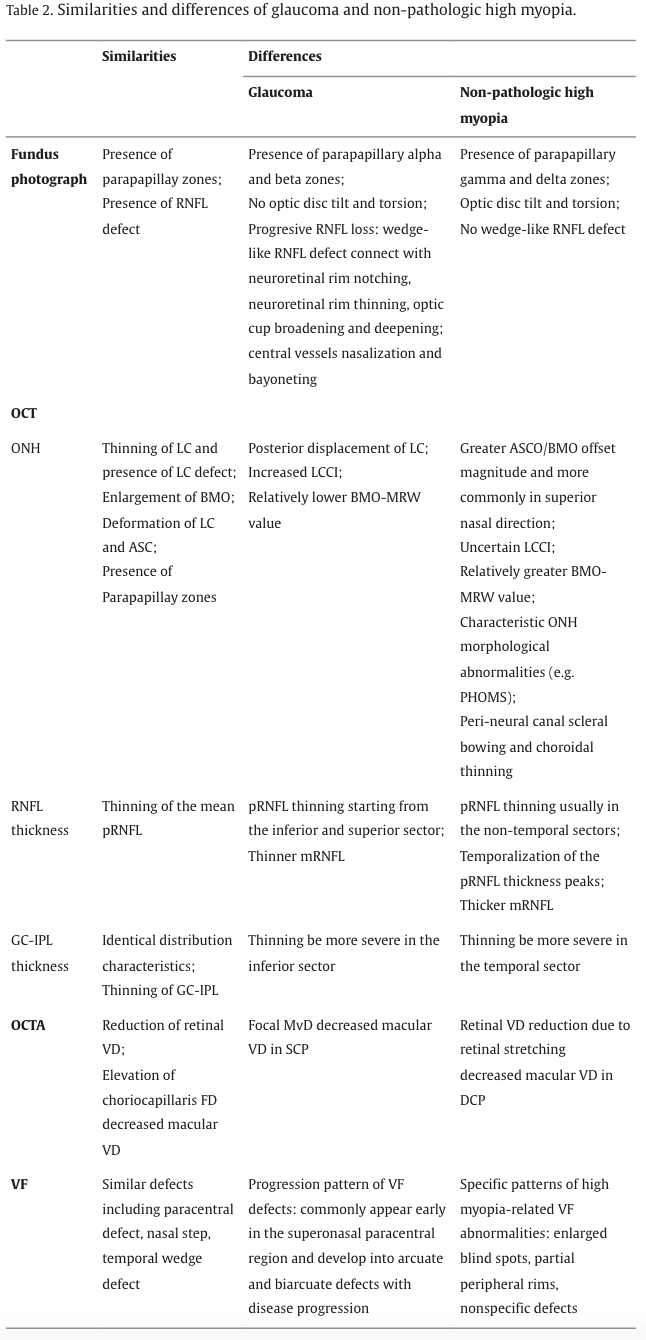
Figure 6 Summary table of similarities and differences in imaging and functional characteristics between high myopia and glaucoma
ZOC has long been committed to tackling clinical challenges that threaten eye health. With the support of the Clinical Research Center at ZOC, a series of studies have been conducted under projects such as the National Key Research and Development Program and the "Dengfeng Plan" for the construction of high-level hospitals in Guangdong Province. In 2019, Professor Xiulan Zhang's team took the lead in collaborating with 13 experts in high myopia, glaucoma, and epidemiology from seven countries to establish the global Glaucoma Suspects with High Myopia study group (GSHM). The group has carried out a series of clinical research projects, aiming to provide solid evidence-based medicine for the early detection, diagnosis, and treatment of patients with high myopia combined with glaucoma. Currently, the team has established a cohort of over 1,600 patients with high myopia combined with glaucoma and has conducted cohort studies and randomized controlled clinical trials based on this cohort. In recent years, the team has published 17 internationally high-level papers related to high myopia, including one in the top journal in ophthalmology, "Progress in Retinal and Eye Research," and two in "Ophthalmology." Among them, the team innovatively proposed a novel classification standard for non-pathologic high myopia-associated visual field defects (Ophthalmology. 2022 Jul;129(7):803-812), established a Chinese database of peripapillary RNFL thickness based on OCT (Ophthalmology. 2023 Dec;130(12):1279-1289) and obtained a patent (Patent No. ZL202111117917.6), and proposed a new classification of optic nerve head structural characteristics in patients with high myopia and explored their correlation with glaucoma-related visual field defects (Asia Pac J Ophthalmol (Phila). 2023 Sep-Oct 01;12(5):460-467). Their work provides valuable clinical references for the early detection, diagnosis, and treatment of patients with high myopia combined with glaucoma.
This article is part of the GSHM series of studies, led by ZOC and completed in collaboration with top international experts in glaucoma and high myopia. It represents another high-quality research achievement resulting from international collaboration at ZOC. The first affiliation of this article is ZOC at Sun Yat-sen University, the State Key Laboratory of Ophthalmology, and the Guangdong Provincial Clinical Research Center for Eye Diseases. Professor Xiulan Zhang, Dr. Jingwen Jiang, and Dr. Kangjie Kong are co-first authors (Figure 7), while Professor Dennis S.C. Lam, Chair of the Department of Ophthalmology and Visual Sciences at The Chinese University of Hong Kong (Shenzhen) and Hong Kong Eye Hospital, is the corresponding author.
This article was co-supervised by Professor Robert N. Weinreb and Professor Linda M. Zangwill from the Shiley Eye Institute at the University of California, San Diego, Professor Jost B. Jonas from the Medical Faculty Mannheim at Heidelberg University in Germany, Professor Kyoko Ohno-Matsui from the Tokyo Medical and Dental University in Japan, and Dr. Timothy P.H. Lin from the Hong Kong Eye Hospital.
Article link:
https://www.sciencedirect.com/science/article/pii/S1350946224000119
返回列表
|