1、Lavine JA, Ramos MS, Wolk AM, et al. Heterogeneity of cultured melanocyte elongation and proliferation factor in bilateral diffuse uveal melanocytic proliferation. Exp Eye Res. 2019, 184: 30-37. DOI: 10.1016/j.exer.2019.04.006Lavine JA, Ramos MS, Wolk AM, et al. Heterogeneity of cultured melanocyte elongation and proliferation factor in bilateral diffuse uveal melanocytic proliferation. Exp Eye Res. 2019, 184: 30-37. DOI: 10.1016/j.exer.2019.04.006
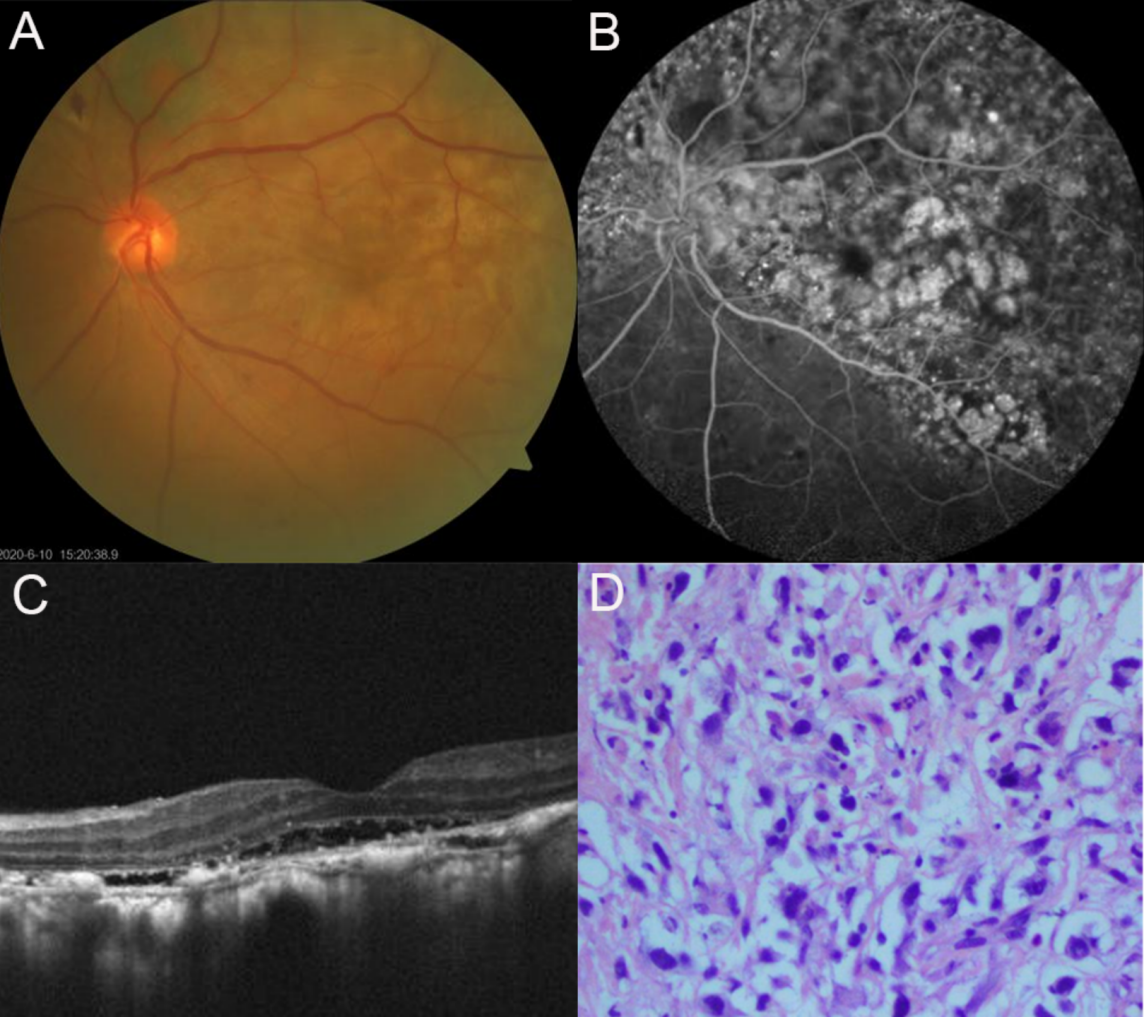
2、Tong N, Wang L, Wang N, et al. Bilateral diffuse uveal melanocytic proliferation secondary to rectal adenocarcinoma: a case report and literature review. Front Med (Lausanne). 2021, 8: 691686. DOI: 10.3389/fmed.2021.691686Tong N, Wang L, Wang N, et al. Bilateral diffuse uveal melanocytic proliferation secondary to rectal adenocarcinoma: a case report and literature review. Front Med (Lausanne). 2021, 8: 691686. DOI: 10.3389/fmed.2021.691686
3、Rafei-Shamsabadi D, Schneider J, Trefzer L, et al. Case report: blurred vision and eruptive nevi - bilateral diffuse uveal melanocytic proliferation with mucocutaneous involvement in a lung cancer patient. Front Oncol. 2021, 11: 658407. DOI: 10.3389/fonc.2021.658407.Rafei-Shamsabadi D, Schneider J, Trefzer L, et al. Case report: blurred vision and eruptive nevi - bilateral diffuse uveal melanocytic proliferation with mucocutaneous involvement in a lung cancer patient. Front Oncol. 2021, 11: 658407. DOI: 10.3389/fonc.2021.658407.
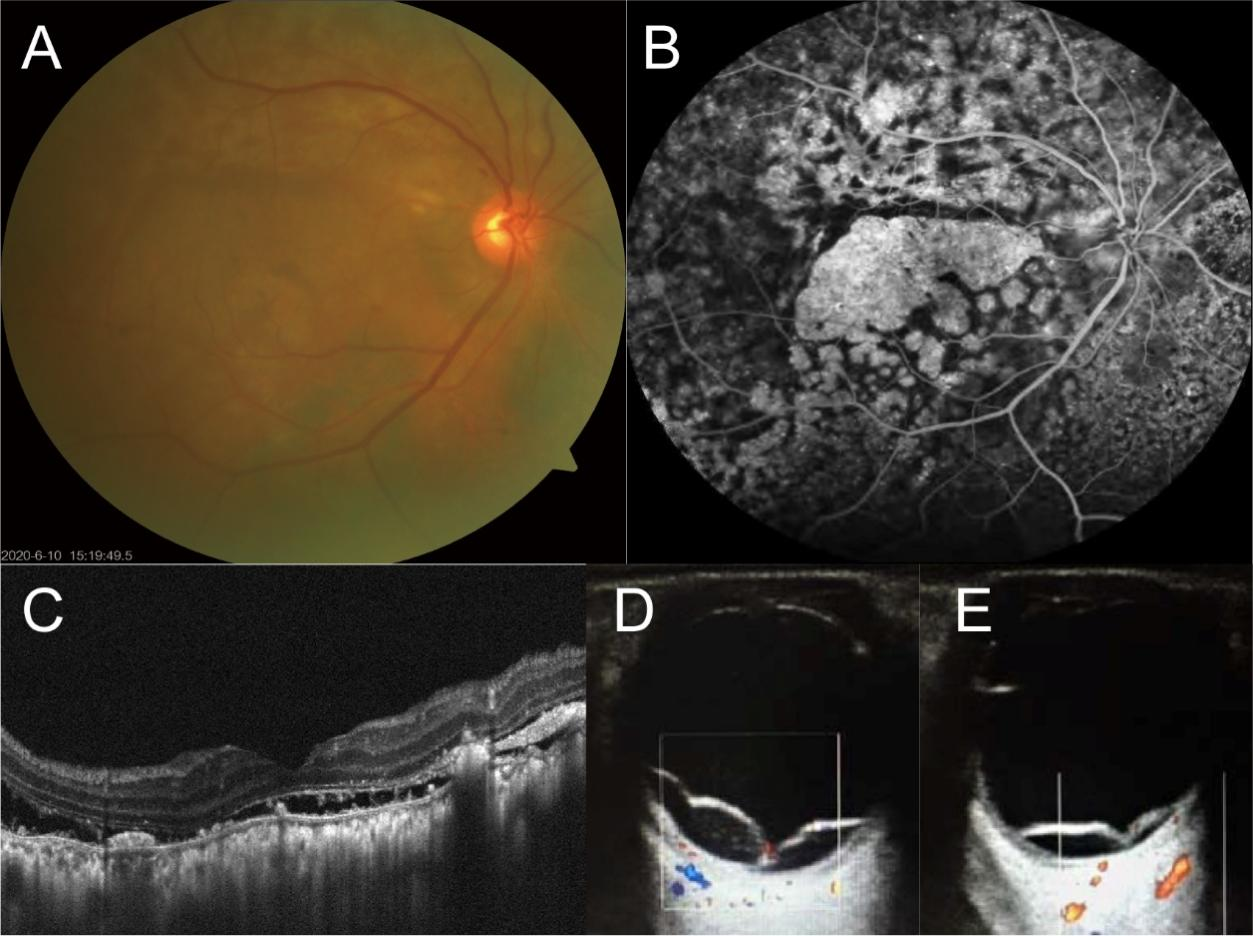
4、Guo J, Tang W, Liu W, et al. A case report of ultrasonographic findings in bilateral diffuse Uveal melanocytic proliferation. BMC Ophthalmol. 2020, 20(1): 476. DOI: 10.1186/s12886-020-01720-6.Guo J, Tang W, Liu W, et al. A case report of ultrasonographic findings in bilateral diffuse Uveal melanocytic proliferation. BMC Ophthalmol. 2020, 20(1): 476. DOI: 10.1186/s12886-020-01720-6.
5、Weppelmann TA, Khalil S, Zafrullah N, et al. Ocular paraneoplastic syndromes: a critical review of diffuse uveal melanocytic proliferation and autoimmune retinopathy. Cancer Control. 2022, 29: 10732748221144458. DOI: 10.1177/10732748221144458.Weppelmann TA, Khalil S, Zafrullah N, et al. Ocular paraneoplastic syndromes: a critical review of diffuse uveal melanocytic proliferation and autoimmune retinopathy. Cancer Control. 2022, 29: 10732748221144458. DOI: 10.1177/10732748221144458.
6、Parakh S, Maheshwari S, Das S, et al. Presumed bilateral diffuse uveal melanocytic proliferation - A case report and review of literature. Am J Ophthalmol Case Rep. 2022, 27: 101582. DOI: 10.1016/j.ajoc.2022.101582. Parakh S, Maheshwari S, Das S, et al. Presumed bilateral diffuse uveal melanocytic proliferation - A case report and review of literature. Am J Ophthalmol Case Rep. 2022, 27: 101582. DOI: 10.1016/j.ajoc.2022.101582.
7、 Ryu C, Havens SJ, Chen J, et al. A case of bilateral diffuse uveal melanocytic proliferation followed by massive unilateral uveal proliferation. Ocul Immunol Inflamm. 2024, 32(10): 2605-2611. DOI: 10.1080/09273948.2024.2355577. Ryu C, Havens SJ, Chen J, et al. A case of bilateral diffuse uveal melanocytic proliferation followed by massive unilateral uveal proliferation. Ocul Immunol Inflamm. 2024, 32(10): 2605-2611. DOI: 10.1080/09273948.2024.2355577.
8、Ayachit G, Ayachit A, Joshi S, et al. A rare case of unilateral diffuse melanocytic proliferation. Indian J Ophthalmol. 2018, 66(4): 588-590. DOI: 10.4103/ijo.IJO_979_17.Ayachit G, Ayachit A, Joshi S, et al. A rare case of unilateral diffuse melanocytic proliferation. Indian J Ophthalmol. 2018, 66(4): 588-590. DOI: 10.4103/ijo.IJO_979_17.
9、 Joseph A, Rahimy E, Sarraf D. Bilateral diffuse uveal melanocytic proliferation with multiple iris cysts. JAMA Ophthalmol. 2014, 132(6): 756-760. DOI: 10.1001/jamaophthalmol.2014.311. Joseph A, Rahimy E, Sarraf D. Bilateral diffuse uveal melanocytic proliferation with multiple iris cysts. JAMA Ophthalmol. 2014, 132(6): 756-760. DOI: 10.1001/jamaophthalmol.2014.311.
10、 Kalogeropoulos D, Afshar F, De Salvo G, et al. Diagnostic and therapeutic considerations in patients with bilateral diffuse uveal melanocytic proliferation. Int Ophthalmol. 2024, 44(1): 149. DOI: 10.1007/s10792-024-03087-9. Kalogeropoulos D, Afshar F, De Salvo G, et al. Diagnostic and therapeutic considerations in patients with bilateral diffuse uveal melanocytic proliferation. Int Ophthalmol. 2024, 44(1): 149. DOI: 10.1007/s10792-024-03087-9.
11、De Salvo G, Prakash P, Rennie CA, et al. Long-term survival in a case of bilateral diffuse uveal melanocytic proliferation. Eye (Lond), 2011, 25(10): 1385-1386. DOI: 10.1038/eye.2011.180. De Salvo G, Prakash P, Rennie CA, et al. Long-term survival in a case of bilateral diffuse uveal melanocytic proliferation. Eye (Lond), 2011, 25(10): 1385-1386. DOI: 10.1038/eye.2011.180.
12、Jansen JCG, Van Calster J, Pulido JS, et al. Early diagnosis and successful treatment of paraneoplastic melanocytic proliferation. Br J Ophthalmol. 2015, 99(7): 943-948. DOI: 10.1136/bjophthalmol-2014-305893. Jansen JCG, Van Calster J, Pulido JS, et al. Early diagnosis and successful treatment of paraneoplastic melanocytic proliferation. Br J Ophthalmol. 2015, 99(7): 943-948. DOI: 10.1136/bjophthalmol-2014-305893.
13、Sarkar P, Mehtani A, Gandhi HC, et al. Paraneoplastic ocular syndrome: a Pandora’s box of underlying malignancies. Eye (Lond), 2022, 36(7): 1355-1367. DOI: 10.1038/s41433-021-01676-x. Sarkar P, Mehtani A, Gandhi HC, et al. Paraneoplastic ocular syndrome: a Pandora’s box of underlying malignancies. Eye (Lond), 2022, 36(7): 1355-1367. DOI: 10.1038/s41433-021-01676-x.
14、 Borruat FX, Othenin-Girard P, Uffer S, et al. Natural history of diffuse uveal melanocytic proliferation. Case report. Ophthalmology. 1992, 99(11): 1698-1704. DOI: 10.1016/s0161-6420(92)31743-9. Borruat FX, Othenin-Girard P, Uffer S, et al. Natural history of diffuse uveal melanocytic proliferation. Case report. Ophthalmology. 1992, 99(11): 1698-1704. DOI: 10.1016/s0161-6420(92)31743-9.
15、Mihic Góngora L, Santalla C, Contreras Toledo D, et al. Bilateral diffuse uveal melanocytic proliferation (BDUMP) as ocular toxicity from durvalumab in advanced renal carcinoma. Eur J Cancer. 2022, 171: 10-12. DOI: 10.1016/j.ejca.2022.04.037. Mihic Góngora L, Santalla C, Contreras Toledo D, et al. Bilateral diffuse uveal melanocytic proliferation (BDUMP) as ocular toxicity from durvalumab in advanced renal carcinoma. Eur J Cancer. 2022, 171: 10-12. DOI: 10.1016/j.ejca.2022.04.037.
16、 Jabbarpoor Bonyadi MH, Ownagh V, Rahimy E, et al. Giraffe or leopard spot chorioretinopathy as an outstanding finding: case report and literature review. Int Ophthalmol. 2019, 39(6): 1405-1412. DOI: 10.1007/s10792-018-0948-5. Jabbarpoor Bonyadi MH, Ownagh V, Rahimy E, et al. Giraffe or leopard spot chorioretinopathy as an outstanding finding: case report and literature review. Int Ophthalmol. 2019, 39(6): 1405-1412. DOI: 10.1007/s10792-018-0948-5.
17、 Leskov I, Lyon AT, Jampol LM. Diffuse uveal melanocytic proliferation with primary vitreoretinal lymphoma. JAMA Ophthalmol. 2019, 137(7): 834-837. DOI: 10.1001/jamaophthalmol.2019.0905. Leskov I, Lyon AT, Jampol LM. Diffuse uveal melanocytic proliferation with primary vitreoretinal lymphoma. JAMA Ophthalmol. 2019, 137(7): 834-837. DOI: 10.1001/jamaophthalmol.2019.0905.
18、Da Silva MV, Rose K, Krema H. Pigment-induced glaucoma secondary to bilateral diffuse uveal melanocytic proliferation. Eur J Ophthalmol. 2022, 32(1): NP62-NP65. DOI: 10.1177/1120672120953076. Da Silva MV, Rose K, Krema H. Pigment-induced glaucoma secondary to bilateral diffuse uveal melanocytic proliferation. Eur J Ophthalmol. 2022, 32(1): NP62-NP65. DOI: 10.1177/1120672120953076.
19、Zhao F, Hu L, Guo R, et al. Bilateral diffuse uveal melanocytic proliferation initially presented as glaucoma. Ocul Immunol Inflamm. 2023, 31(3): 601-608. DOI: 10.1080/09273948.2022.2032201. Zhao F, Hu L, Guo R, et al. Bilateral diffuse uveal melanocytic proliferation initially presented as glaucoma. Ocul Immunol Inflamm. 2023, 31(3): 601-608. DOI: 10.1080/09273948.2022.2032201.
20、Duong HQ, McLean IW, Beahm DE. Bilateral diffuse melanocytic proliferation associated with ovarian carcinoma and metastatic malignant amelanotic melanoma. Am J Ophthalmol. 2006, 142(4): 693-695. DOI: 10.1016/j.ajo.2006.04.059. Duong HQ, McLean IW, Beahm DE. Bilateral diffuse melanocytic proliferation associated with ovarian carcinoma and metastatic malignant amelanotic melanoma. Am J Ophthalmol. 2006, 142(4): 693-695. DOI: 10.1016/j.ajo.2006.04.059.
21、Miles SL, Niles RM, Pittock S, et al. A factor found in the IgG fraction of serum of patients with paraneoplastic bilateral diffuse uveal melanocytic proliferation causes proliferation of cultured human melanocytes. Retina. 2012, 32(9): 1959-1966. DOI: 10.1097/IAE.0b013e3182618bab. Miles SL, Niles RM, Pittock S, et al. A factor found in the IgG fraction of serum of patients with paraneoplastic bilateral diffuse uveal melanocytic proliferation causes proliferation of cultured human melanocytes. Retina. 2012, 32(9): 1959-1966. DOI: 10.1097/IAE.0b013e3182618bab.
22、Alrashidi S, Aziz AA, Krema H. Bilateral diffuse uveal melanocytic proliferation: a management dilemma. BMJ Case Rep. 2014, 2014: bcr2014204387. DOI: 10.1136/bcr-2014-204387. Alrashidi S, Aziz AA, Krema H. Bilateral diffuse uveal melanocytic proliferation: a management dilemma. BMJ Case Rep. 2014, 2014: bcr2014204387. DOI: 10.1136/bcr-2014-204387.
23、 Schelvergem KV, Wirix M, Nijs I, et al. Bilateral diffuse uveal melanocytic proliferation with good clinical response to plasmapheresis and treatment of the primary tumor. Retin Cases Brief Rep. 2015, 9(2): 106-108. DOI: 10.1097/ICB.0000000000000104. Schelvergem KV, Wirix M, Nijs I, et al. Bilateral diffuse uveal melanocytic proliferation with good clinical response to plasmapheresis and treatment of the primary tumor. Retin Cases Brief Rep. 2015, 9(2): 106-108. DOI: 10.1097/ICB.0000000000000104.
24、Kenney L, Hughes M. Adrenocortical carcinoma: role of adjuvant and neoadjuvant therapy. Surg Oncol Clin N Am. 2023, 32(2): 279-287. DOI: 10.1016/j.soc.2022.10.005. Kenney L, Hughes M. Adrenocortical carcinoma: role of adjuvant and neoadjuvant therapy. Surg Oncol Clin N Am. 2023, 32(2): 279-287. DOI: 10.1016/j.soc.2022.10.005.
25、Puglisi S, Calabrese A, Basile V, et al. New perspectives for mitotane treatment of adrenocortical carcinoma. Best Pract Res Clin Endocrinol Metab. 2020, 34(3): 101415. DOI: 10.1016/j.beem.2020.101415. Puglisi S, Calabrese A, Basile V, et al. New perspectives for mitotane treatment of adrenocortical carcinoma. Best Pract Res Clin Endocrinol Metab. 2020, 34(3): 101415. DOI: 10.1016/j.beem.2020.101415.
26、Hasebe M, Shibue K, Honjo S, et al. Adrenocortical carcinoma. QJM. 2022, 115(1): 43-44. DOI: 10.1093/qjmed/hcab276.Hasebe M, Shibue K, Honjo S, et al. Adrenocortical carcinoma. QJM. 2022, 115(1): 43-44. DOI: 10.1093/qjmed/hcab276.
27、De Filpo G, Mannelli M, Canu L. Adrenocortical carcinoma: current treatment options. Curr Opin Oncol. 2021, 33(1): 16-22. DOI: 10.1097/CCO.0000000000000695. De Filpo G, Mannelli M, Canu L. Adrenocortical carcinoma: current treatment options. Curr Opin Oncol. 2021, 33(1): 16-22. DOI: 10.1097/CCO.0000000000000695.