HIGHLIGHTS
· The Vision Centre (VC) model pioneered by Aravind Eye Care System has enabled scalable, sustainable delivery of primary eye care in underserved rural regions.
· In 2023–2024, the network of 113 VCs recorded nearly 1 million outpatient visits, achieved 25% population coverage, and generated cost savings of ₹647 million (US$7.8 million) for patients.
· The model demonstrated high rates of compliance: 70% for tertiary referrals and 72% for advised cataract surgeries.
· Integration of digital tools—electronic medical records, fundus imaging, and live teleophthalmology—enabled remote diagnosis and continuity of care.
· Use of artificial intelligence for diabetic retinopathy screening improved diagnostic efficiency and reduced dependency on human graders.
· The model has been successfully scaled to other Indian states and replicated in countries like Bangladesh, Kenya, and Nigeria.
· With proper adaptation, the VC framework holds potential to help low- and middle-income countries (LMICs) achieve WHO’s 2030 eye health targets for effective cataract surgery and refractive error coverage.
· Future directions include expanding AI applications, enhancing staff training, and strengthening government-NGO partnerships to integrate VCs into national health systems.
INTRODUCTION
Achieving universal eye health remains an elusive global challenge, particularly in low-and middle-income countries where a disproportionate burden of visual impairment and blindness persists [1]. Despite remarkable advances in tertiary eye care, access to primary eye care remains a major challenge in rural and underserved regions, where most of the population resides [2,3]. The disparity underscores the need for innovative scalable models that bridge the gap in accessibility, affordability, and quality of eye care services between healthcare infrastructure and communities in need.
India is home to the world’s largest population of people with avoidable blindness, approximately 8 million individuals [4]. While efforts have improved cataract surgical rates (currently 6,000 per million population), the prevalence of blindness continues to rise due to an aging population, lack of a comprehensive eye care approach, and weak primary eye care systems [2,5,6]. In India, approximately 65-70% of the population resides in rural areas, where access to eye care remains limited. The prevalence of blindness and visual impairment is significantly higher in rural regions, with cataract, uncorrected refractive errors, and diabetic retinopathy being the leading causes [2,4,5]. National surveys have shown that rural populations bear nearly twice the burden of avoidable blindness compared to urban counterparts [6].
The government’s National Program for Control of Blindness (NPCB) has sought to strengthen PEC networks through primary health centres and community centres, but challenges in implementation persist [7]. To bridge this gap, non-governmental organizations have established Vision Centres (VCs) as part of their primary eye care networks [8]. Operating in alignment with NPCB’s objectives, VCs provide primary eye care in rural areas, staffed by locally recruited, trained technicians who deliver core services such as refraction, spectacle dispensing, diagnosis of common eye conditions, and referrals for advanced care. These models demonstrate diverse approaches to enhancing access to eye care, yet variability exists in their technological integration, financial models, and long-term sustainability.
Building on this landscape, the Vision Centre Model, pioneered by the Aravind Eye Care System (AECS) [8,9] exemplifies an innovative approach to eye care service delivery. Designed to provide comprehensive primary eye care services at the grassroots level, AECS VCs operate as permanent facilities, staffed by allied ophthalmic personnel (AOP) and supported by digital technologies and teleophthalmology link to base hospitals. By integrating technology, community engagement and affordable care, the model bridges gaps in access, affordability and quality, while highlighting its potential to achieve universal eye health coverage. These centres provide a full spectrum of services from basic eye examinations and refractive error correction to treatment for common ocular conditions (eye infections, dry eyes, minor ocular trauma) as well as an accountable referral mechanism for services that can only be delivered in secondary or tertiary level facilities.
Importantly, the VC model aligns with global health priorities and the Sustainable Development Goals (SDGs) [10]. By ensuring equitable access to quality eye care, the model contributes to SDG 3 (Good Health and Well-being) and SDG 1 (No Poverty) while addressing key components of Universal Health Coverage (UHC). The World Health Organization’s “World Report on Vision” (2019) underscores the critical role of integrating eye care into primary healthcare systems to achieve UHC [1].
This review explores the evolution, implementation and impact of the digital technology integrated AECS VC model, with a focus on its potential to serve as a blueprint for universal eye health. By analysing the model’s technological innovations, operational sustainability, and alignment with global health priorities, the article highlights its role in bridging the gap between need and access in primary eye care.
AECS VISION CENTRE MODEL: OVERVIEW AND DESIGN
Origin and Development of the Vision Centre Model
The Vision Centre (VC) model was conceived and developed by the AECS (www.aravind.org) in Tamil Nadu, India as a response to the critical need for accessible, affordable, and high-quality primary eye care. Initiated in 2004, the model aims to address the high prevalence of avoidable blindness in rural and underserved communities, where eyecare resources are scarce, and systematic barriers prevent timely intervention. Vision Centres are set up in areas that have no eye care services within 10-15 KM radius [9]. In such areas, Vision Centres are set-up in small rural towns with a population of 10,000 and serves surrounding villages within a radius of 5 to 8 KM, covering a population of 50,000 to 75,000.
Objectives and Key Components of the Model
The VC model has three primary objectives: improving access to comprehensive eye care, making care affordable, and ensuring sustainability. Its key components include the integration of digital technology, deployment of trained allied ophthalmic personnel (AOP) and strong focus on quality and closing the care loop.
Digital Technology Integration
The VC model leverages teleconsultation and digital health technology to bridge the gap between patients and ophthalmologists. Each vision centre has two computers, internet connectivity and an electronic medical record (EMR) system. This facilitates real-time sharing of clinical data and live video-consultation for every patient with an ophthalmologist at the base hospital. All Vision Centres have Fundus cameras and anterior segment imaging capabilities as well. These images are posted in the EMR and this enables remote diagnosis of conditions like diabetic retinopathy and glaucoma [11]. In addition, the retinal images from the fundus cameras are integrated with Artificial Intelligence algorithm to detect DR at an early stage [12,13]. These advancements ensure timely diagnosis of complex conditions even in the most remote locations. The digital technologies are also utilized for supply chain, financial and overall management of the VCs.
Human Resource Deployment
Central to the VC model is the training and empowerment of AOPs who serve as the backbone of operations. AOPs are rigorously trained to conduct comprehensive eye examinations using a slit lamp, measure intraocular pressure using applanation tonometer, perform subjective refraction, and arrive at preliminary diagnoses. This strategic task-shifting ensures that ophthalmologists need to be involved only to verify the AOPs findings and for advanced care, thus ensuring diagnostic quality[14]. Each VC is staffed with two AOPs: 1) Vision Technician (VT) who would be a skilled refractionist with a minimum of two years of experience at the base hospital. Prior to posting to Vision Centre, they undergo six month-long intensive training to acquire competencies such as comprehensive eye examination using slit lamp, fundus examination with a direct ophthalmoscope, taking fundus images, measuring intraocular pressure, identifying eye conditions, checking vital signs and entering all the findings in the EMR. 2) VC Coordinator (VCC) who, by training, would be an outpatient ophthalmic assistant with a minimum two years of experience at the base hospital. Similar to the VTs, the VCCs also are provided an intensive training in spectacle dispensing, patient counselling, medical records management, pharmacology, accounting and stock maintenance. Skill evaluation and continues medical education programmes are conducted once every six months to ensure that the staff are up to date with their knowledge, skills and competencies.
Infrastructure and Operational Workflow
Each VC is equipped with state-of-the-art diagnostic tools, such as slit lamp, autorefractor, applanation tonometer and fundus camera. The operational workflow is streamlined to include patient registration visual acuity testing, subjective refraction, slit lamp examination and digital imaging. Images and clinical data are entered in the cloud-based EMR for simultaneous review by the tele-ophthalmologist, thus enabling accurate and timely diagnoses [8].
The full scope of clinical services provided at a VC is described in Table 1. In brief, VCs manage a range of common ocular conditions, including refractive errors, cataract, diabetic retinopathy, glaucoma and ocular surface infections. Spectacles and essential medications are dispensed on-site, and minor procedures such as foreign body removal are performed by trained vision technicians. Initial screening and diagnosis are supported by slit lamp examination, subjective refraction, intraocular pressure measurement and fundus imaging. Referrals are arranged and followed up for advanced examinations or surgical care as needed.
Service quality is ensured through standardized clinical and operational audits conducted across all VCs, along with systematic daily collection of patient feedback. Performance metrics, such as refraction accuracy, referral compliance, and turnaround time, are regularly monitored to maintain high standards of care. By combining technological innovation, skilled human resources, and patient-centred processes, the VC model exemplifies a scalable and sustainable solution to achieving universal eye health.
Table 1 Scope of Clinical Services at a Vision Centre
|
|
Case Finding
|
Interventions
|
Follow-up
|
|
Preventive
|
Curative
|
Referral
|
|
Cataract
|
√
|
|
|
√
|
√
|
|
Ref. Error
|
√
|
|
√
|
|
√
|
|
Childhood Blindness
|
√
|
√
|
|
√
|
√
|
|
Diabetic Retinopathy
|
√*
|
|
|
√
|
√
|
|
Glaucoma
|
√*
|
|
|
√
|
√
|
|
Cornea
|
√
|
√
|
√
|
√
|
√
|
|
Trachoma
|
√
|
√
|
√
|
√
|
√
|
|
Low Vision
|
√
|
|
|
√
|
√
|
*Supported by artificial intelligence or remote specialist
TECHNOLOGICAL INNOVATIONS IN THE VISION CENTRE MODEL
The VC model demonstrates how technological innovations can bridge gaps in healthcare delivery, particularly in underserved regions. By leveraging cutting-edge tools and systems, VCs have democratized eye care, making it very accessible, affordable, efficient, and effective.
Role of Teleophthalmology in Connecting Vision Centres to Base Hospitals
A cornerstone of the VC model is its seamless integration of teleophthalmology, enabling real-time consultations between patients at remote VCs and ophthalmologists at base hospitals. Teleconsultation platforms facilitate diagnosis and treatment recommendations for conditions requiring specialized care. Telemedicine has a pivotal role in enhancing the reach of eye care services, particularly for complex cases like diabetic retinopathy or glaucoma, which often require expert evaluation [11].
Conditions that require specialist consultation are referred to the base hospital and followed-up. Teleophthalmology not only ensures timely interventions but also reduces the need for travel, thereby enhancing affordability and patient satisfaction. The sustained use of teleconsultation in VCs is supported by stable internet connectivity, EMR integration, dedication IT support, and user-friendly platforms. Routine use is further enabled through streamlined workflows and regular staff training in digital tools.
Integration of Electronic Medical Records (EMRs)
The adoption of EMR has revolutionized patient data management within the VC framework. EMR streamline patient registration, history-taking, and follow-up, ensuring that accurate records are maintained for every individual. EMR also enables longitudinal tracking of patient outcomes, facilitating data-driven decision-making at both the micro and macro levels [14]. By linking VCs to the central database at base hospitals, EMRs contribute to coordinated care, reducing redundancies and improving efficiency. The digital patient database also allows tracking of coverage at village level and gives insights on community’s health seeking behaviour.
Use of Diagnostic Tools and Artificial Intelligence in Screenings
Advancements in diagnostic tools and artificial intelligence (AI) have significantly augmented the VC model's capabilities. Portable fundus cameras, and AI-based systems for disease detection are now integral to VCs. In a validation study involving nearly 10,000 retinal images, the AI algorithm used for diabetic retinopathy screening in the AECS VCs demonstrated a sensitivity of 90.3% (95% CI, 87.5%–92.7%) and specificity of 98.1% (95% CI, 97.5%–98.5%) for detecting referable DR [12], This ensures that the at-risk individuals are promptly identified. AI integration, in general, has been reported to have reduced dependence on human graders, improving diagnostic turnaround times [9, 13]. Furthermore, the use of portable diagnostic tools ensures that even patients in remote locations can access high-quality eye care.
Impact of Technology on Service Delivery and Efficiency
The cumulative impact of technological innovations in the VC model is evident in its enhanced service delivery and operational efficiency. Teleophthalmology, EMR, and AI not only expand the scope of services provided at VCs but also ensure cost-effectiveness by optimizing resource allocation. For instance, teleconsultations reduce the burden on tertiary care facilities and patients, by managing non-critical cases locally. Similarly, AI-driven tools minimize diagnostic delays, enabling timely treatment. Technology integration in VCs aligns seamlessly with the principles of universal health coverage by addressing barriers related to access, quality, and affordability (17).
By leveraging technology, VCs have evolved into dynamic hubs of primary eye care, effectively meeting the needs of diverse populations. These innovations have not only strengthened the VC model but also set a precedent for adopting technology-driven approaches in other primary healthcare domains.
IMPACT OF THE VISION CENTRE MODEL
AECS envisioned VCs as a localized, community-based solution that could operate independently while being integrated into a larger network, including tertiary care hospitals to enable an accountable, robust, referral mechanism. This VC model has emerged as a transformative force in the delivery of primary eye care, particularly in underserved and rural regions. The model has since grown to a network of 113 centres, covering a population of over 10 million, thus demonstrating scalability and replicability. Its impact is multifaceted, going beyond accessibility to health equity and measurable improvements in eye health outcomes.
Improved Accessibility and Utilization of Services
The performance of Vision Centres during the fiscal year 2023-24 highlights their critical role in delivering primary eye care services and bridging the gap in community health. Table 2 provides an overview of the annual patient volumes at the vision centres. The network comprised 113 VCs and recorded a total of 996,567 outpatient visits. This included 535,509 new outpatients of which 28% (151,406) were from outside the designated services areas and 461,058 returning outpatients with 27% (124,008) coming from outside the service areas. Toward addressing refractive errors, 146,489 spectacles were prescribed of which 79% (115,626) were purchased directly at the centres. The VCs advised 54,748 patients for cataract surgeries, with 72% (39,274) of them accepting surgical intervention at the base hospitals. Although the immediate post-operative follow-up happens at the base hospital, the routine follow-up consultations for uneventful cases can be organized at the VCs. Additionally, 73,843 patients were referred to the base hospital for speciality care, such as for the management of diabetic retinopathy and glaucoma, of which 70% (51,406) complied with the referral and sought care at the tertiary base hospital. Default tracking is done via phone calls; social factors are identified as key barriers for compliance.
These measures along with the cumulative figures (Table 2b) highlights the reach and efficiency of Vision Centres in providing essential eye care services. Of particular note is the population coverage rate of 25% reflecting the program’s success in meeting the eye health needs of underserved areas. Additionally, a significant proportion of patients come from outside the designated service area, underscoring the reputation and accessibility of Vision Centres as a trusted source of care.
|
No of Vision Centres
|
113
|
|
New Outpatients
|
*535,509
|
|
Review Outpatients
|
**461,058
|
|
Total Outpatient visits
|
996,567
|
|
Spectacles - Prescribed
|
146,489
|
|
- Purchased (78%)
|
115,626
|
|
Cataract surgeries - Advised
|
54,748
|
|
- Accepted (68%)
|
39,274
|
|
Specialty - Referrals to base hospitals
|
73,843
|
|
- Compliance (68%)
|
51,406
|
|
* Includes 151,496 (28%) New patients from outside the service area
** Includes 124,008 (27%) Review patients from outside the service area
|
Table 2b: Cumulative patient volumes since inception till March -2024
|
No of Vision Centres
|
113
|
|
Population covered
|
12 million
|
|
New outpatients (Unique patients)
|
*3,049,827
|
|
Review outpatients
|
**2,296,508
|
|
Total outpatient visits (all)
|
7,782,549
|
|
Population coverage (unique patients)
|
25%
|
|
Spectacles delivered
|
987,676
|
|
Cataract surgeries
|
273,937
|
|
* Excludes 1,486,351 (33%) New patients from outside the service area
**Excludes 949,863 (29%) Review patients from outside the service area
|
Cost Savings and Economic Impact of Vision Centres
The VC model offers a significant financial advantage to patients by drastically reducing the cost of accessing eye care services. Compared to visiting base hospitals, patients save approximately INR 650 (US$9) per visit by utilizing Vision Centres (Table 3). This savings arises from reduced transport costs, lower incidental expenses, and minimized lost wages. The model's accessibility further alleviates the need for patient attendants, leading to additional indirect cost reductions.
Table 3 Comparison of Expenses: Base Hospital vs Vision Centre
|
Expense Category
|
Base Hospital
(INR)
|
Vision Centre
(INR)
|
Savings per patient
|
|
INR
|
|
Transport
|
140
|
45
|
95
|
|
Other expenses
|
240
|
60
|
180
|
|
Lost wages
|
600
|
225
|
375
|
|
Total
|
980
|
330
|
(US$ 9) 650
|
In the fiscal year 2023-24, nearly one million outpatients benefited from these cost-effective services, resulting in cumulative savings of INR 647 million (US$7.8 million). This substantial economic impact highlights the model's capacity to lower financial barriers to care, particularly for underserved populations. The Vision Centre’s strategic placement in communities ensures that patients spend less time and money traveling to distant base hospitals. By offering comprehensive eye care services locally, Vision Centres not only enhance affordability but also improve convenience, thereby fostering greater patient compliance and continuity of care.
These financial benefits underscore the Vision Centre model’s alignment with principles of Universal Health Coverage (UHC). By making quality eye care services accessible and affordable, Vision Centres contribute to achieving equitable healthcare outcomes while significantly mitigating the economic burden on individuals and families [2]. This approach serves as a scalable and sustainable template for primary eye care delivery in low-resource settings globally [16].
EXPANSION AND SCALING UP OF VISION CENTRES
The VC model has demonstrated remarkable scalability, extending its reach both within and beyond the Aravind Eye Care System. Internally, AECS manages VCs that collectively cover a population of 10 million. Beyond its network, AECS's initiatives have supported eye care programs within India as well as in the neighbouring country – Bangladesh.
Scaling Within India
AECS has worked with the provincial (state) governments and successfully replicated the model across multiple Indian states, showcasing its adaptability to diverse regional needs. This includes 40 VCs established in the state of Tripura, 12 in Chhattisgarh and 32 in Tamil Nadu.
Partnerships in Bangladesh
In Bangladesh, the Vision Centre model has been embraced through partnerships with organizations like BRAC and the Ministry of Health, Government of Bangladesh. As a result, 25 VCs have been established through BRAC in various parts of the country. The Govt. of Bangladesh has already established 200 VCs which is envisioned to provide permanent access to eye care close to 40% of its population. Their plan is to extend this to cover the entire country. The Bangladeshi government’s approach has been to integrate technology-enabled Vision Centres embedded within Upazila (subdistrict) Health Complexes. Key factors in this success include leadership orientation, stakeholder buy-in, and the training of nurses as Vision Technicians (VTs).
Global Expansion
Through its training, consulting and advocacy wing, the Lions Aravind Institute of Community Ophthalmology (LAICO), AECS has initiated a collaborative capacity building programme to assist eye care providers in establishing and enhancing eye care delivery through VCs. This initiative has supported 26 eye hospitals across Kenya, Nigeria, Nepal and India to either by establishing new VCs or enhancing the effectiveness of existing VCs.
It is noteworthy to recognize that about 130 of the low- and middle-income countries (LMICs) have a population of under 15 million, with inadequate eye care [1, 17]. This is comparable to the population currently covered by the AECS VC network (10+ million). The AECS Vision Centre model has proven to be both sustainable and replicable, bridging the gap in primary eye care and making significant strides toward universal eye health. If this model is effectively replicated in these LMICs, it could achieve 100% eye care coverage in these counties.
CHALLENGES AND LESSONS LEARED
Building Community Trust and Increasing Footfalls
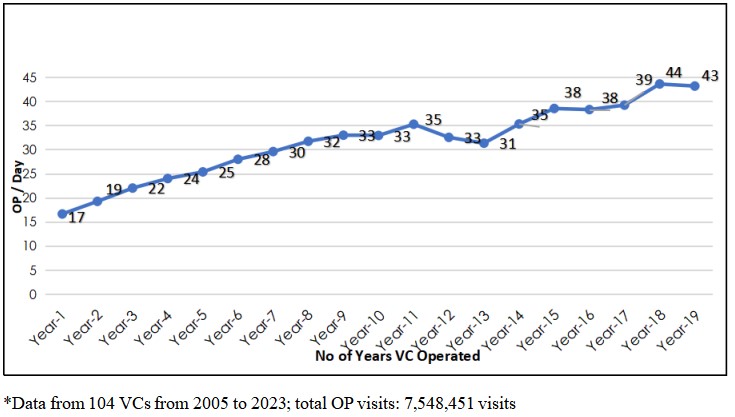
One of the primary challenges faced during the initial set-up of Vision Centres is gaining the trust of the local community and encouraging patient visits. Many people in underserved areas are hesitant to access services due to a lack of awareness or mistrust in new facilities. This issue is mitigated through field interventions to raise awareness abohealthcare ut eye care, actively involving community stakeholders such as local leaders and influencers, and leveraging the experiences of satisfied patients to serve as advocates for the Vision Centre. Long term trust and engagement are built through consistent, high-quality caregiving and strong community relationships. This is evident in the steady increase in average patient visits per VC per day. Growing from 17 patients in the first year (2005) to 43 patients per day by 2023 (Figure 1).
Figure 1 Trend of average outpatient visit per day by age of VC
Recruitment and Retention of Competent Clinical Staff
Ensuring that VCs are staffed with competent clinical staff is another critical challenge. Recruiting staff locally is preferable to ensure operational stability and connection with the community, but finding qualified candidates locally could be challenging. Mitigation strategies include identifying candidates who belong to the VC area from among the base hospital staff, orienting these candidates through a comprehensive training program to equip them with necessary clinical and operational skills and conducting periodic skill assessments and refresher training to ensure their proficiency remains up-to-date.
Dependence on Base Hospitals for Operational Support
VCs rely heavily on base hospitals for supplies, tele-consultation services, referral management, and crisis resolution in situations such as unexpected staff absenteeism, technical failures or patient related emergencies. The seamless functioning of each VC also depends on uninterrupted internet access, stable tele-consultation connectivity and consistent functioning of the EMR system. Ensuring this level of operational continuity requires that the base hospital teams are well-oriented to the objectives and workflows of the VCs. Engaged leadership at the base hospital level is critical to fostering alignment, proactively addressing challenges, and prioritizing the needs of the VCs within the broader eye care delivery system.
Lessons Learned and Recommendations
Sustainable Funding Models: Establishing partnerships with donors, non-governmental organizations, and government agencies towards establishment of VCs helps ensuring financial sustainability and scaling up operations. AECS VCs follow financially self-sustaining model post-initial set up, with operational costs covered by service revenues. However, external funding can support expansion of the network.
Community-Centric approaches: Recruitment and training strategies focused on local candidates enhance community trust and ensure smoother operations.
Continuous Quality Improvement: Implementing regular assessments and providing skill enhancement opportunities for staff ensures high quality care delivery and adaptability to evolving healthcare needs.
Leadership Involvement: The commitment and engagement of leadership at both the base hospital and Vision Centre levels have been pivotal in ensuring goal alignment and facilitating smooth operational workflows. By fostering an enabling environment, organizational leadership has significantly contributed to the model's overall success.
Denominator driven demand generation approach: The VC model at Aravind followed a ‘denominator driven’ approach – focussing on the eye care need of the community rather than that of those who proactively seek care (numerator). This strategy of reaching out to the unreached has been crucial for the successful functioning of each VC and expansion of the VC network within AECS to the current scale and in replicating the model elsewhere within and beyond India.
Closing the care loop: Operational data shows that 85% of patients visiting the VCs leave with a solution, whether it is a diagnosis, spectacles, medicines or treatment for minor conditions. For the remaining 15%, a responsible referral system ensures they receive the necessary care. As a result, every patient benefit from the system, which has been a key factor in building trust, as well as sustaining and growing demand for VC services (Figure 1)
CONCLUSION
The Vision Centre model represents a ground-breaking approach to primary eye care, effectively addressing the challenges of accessibility, affordability, and quality in rural India. In addition to the ACES model, several other VC initiatives have been implemented across different parts of India[2], offering varying levels of service delivery. However, there remains significant scope to enhance these models through the provision of comprehensive eye care and improved population coverage, as exemplified by the AECS VC model. Through the integration of innovative technologies such as teleophthalmology, AI-driven diagnostics, and EMRs, the model has significantly improved eye care delivery in underserved regions. Additionally, its alignment with global health priorities, such as SDG 3 (Good Health and Well-being) and the goal of Universal Health Coverage, underscores its potential to contribute to global efforts toward achieving universal eye health.
At the Seventy-Fourth World Health Assembly in May 2021, WHO Member States endorsed two new ambitious global eye care targets for 2030: a 30-percentage point increase in effective cataract surgery coverage (eCSC), and a 40-percentage point increase in effective refractive error coverage (eREC) [18]. For the first time WHO has recommended a threshold of visual acuity less than 6/12 for intervention and an outcome of 6/12 or better to define effective intervention. These indicators and related targets are intended to drive increases in eye care coverage while delivering high quality care. The VC model has demonstrated its impact through improved access to services, substantial cost savings for patients, and enhanced operational sustainability. This can be the ideal approach for achieving WHOs global eye care targets.
However, challenges related to community engagement, staff recruitment, and dependence on base hospitals remain. By continuing to address these issues and expanding the reach of VCs, this model has the potential to serve as a scalable solution for universal eye health, not only in India but in other resource-limited settings globally. Future research and continued investment in technology, human resources, and sustainable funding are essential to expanding the reach and impact of the VC model. With these efforts, the Vision Centre model can play a critical role in reducing avoidable blindness and ensuring equitable access to eye care worldwide.
Correction notice
None
Acknowledgement
None
Author Contributions
(I) Conception and design: Sanil Joseph & Thulasiraj Ravilla
(II) Administrative support: Thulasiraj Ravilla & Mohammed Gowth
(III) Provision of study materials or patients: Sanil Joseph & Mohammed Gowth
(IV) Collection and assembly of data: Sanil Joseph, Thulasiraj Ravilla & Mohammed Gowth
(V) Data analysis and interpretation: Sanil Joseph and Thulasiraj Ravilla
(VI) Manuscript writing: All authors
(VII) Final approval of manuscript: All authors
Conflict of Interests
None of the authors has any conflicts of interest to disclose. All authors have declared in the completed the ICMJE uniform disclosure form.
Patient consent for publication
None
Ethical Statement
None
Provenance and Peer Review
This article was a standard submission to our journal. The article has undergone peer review with our anonymous review system.
Data Sharing Statement
None
Open Access Statement
This is an Open Access article distributed in accordance with the Creative Commons AttributionNonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license).